Author(s): Mouna EL Ghazi*, Houda Ichihashi, Meryem Zero, Zakaria Ploughman, Fahd Bennani Smires, El Khalifa Sidi Mohamed and Mohamed Chemsi
In-flight incapacitation is a concept that reflects a physiological or psychological maladjustment to the aeronautical environment that will lead to a polymorphic symptomatology which reflects functional dysregulations dominated by neurovegetative imbalance. This is a retrospective study including 9 aircrew, both civilian and military, among 18 having presented an In-flight incapacitation.
The analysis of the different explorations of the Autonomic Nervous System allowed to individualize several autonomic profiles concluding to an autonomic cause of the malaise. The aeronautical constraints whose effects can interfere with the neurovegetative balance will be discussed. This study shows the importance of the Autonomic Nervous System in the genesis of flight incapacitation. Hence the interest to explore it, in aircrew presenting this type of incapacitation.
Flight safety (FS) has always been and remains the prime concern of aviation medicine. The aeronautical world recognizes the enormous progress that has been made in enabling human to reach high altitudes, using increasingly high-performance aircraft. As a result, aeronautical constraints are having a more marked effect on the functioning of the autonomic nervous system, affecting crew performance and potentially leading to in-flight incapacitation (IFI) involving FS. IFI is a concept that reflects a physiological or psychological maladaptation to the aeronautical environment, resulting in a polymorphous symptomatology testifying to functional dysregulations dominated by neurovegetative imbalance [1].
Hence the importance of exploring the autonomic nervous system (ANS), in search of a dysautonomic terrain that may favor the onset of IFI, after ruling out other organic etiologies.
This was a retrospective study carried out between January 2017 and December 2022, which included 9 aircrew, both civilian and military, among 18 FNs who had presented with an IFI. The purpose of studying the ANS using EWING’s cardiovascular reactivity tests was to confirm the dysautonomic nature of the MEV, after an etiological assessment that revealed no organic cause that could explain the IFI [2-4].
It should be noted that these tests were not performed on a single hostess in whom the dysautonomic origin of her malaise was identified clinically (micturition syncope).
The primary objective of this study is to determine the autonomic profile of aircrew presenting with IFI and whose conventional etiological investigation is negative.
The secondary objective is to identify the different forms of autonomic dysregulation that can trigger IFI and their impact on fitness.
Patients included in this study presenting an IFI from January 2017 to December 2022, and whose conventional etiological investigation had not found any cause.
aircrew presenting with IFI whose etiological investigation found a non-dysautonomic cause of malaise, including a positive urine toxicology test (cannabis, cocaine, amphetamines and opiates).
Among the 9 cases of IFI reported, 7 were loss of consciousness, including 2 losses of consciousness under load factor (G-LOC), and 2 tachycardia attacks.
The specialty breakdown of aircrew presenting with IFI is shown in Table 1.
|
Speciality |
Numbers |
||
|
stewardess |
5 |
5 |
|
|
Pilots |
Fighter pilot |
2 |
4 |
|
commercial pilot |
1 |
|
|
|
Military transport pilot |
1 |
|
|
In our study, we found that 4 aircrew (50%) had already suffered at least one IFI in the course of their career. In addition, 2 stewardesses were being monitored for thyroid nodules in euthyroid, and one of them, as well as the fighter pilot, had a history of vagal malaise on the ground. The military transport pilot was diabetic type 2.
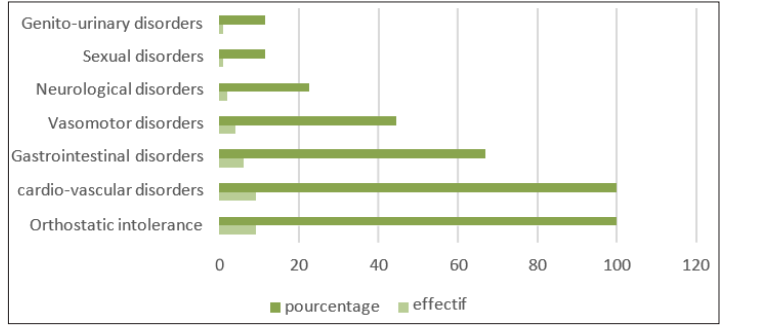
Figure 1: Distribution of Patients According to Functional Dysautonomia Signs
In our population, all aircrew had orthostatic intolerance and cardiovascular disorders as functional signs of dysautonomia.
In addition, 6 had gastrointestinal disorders, 4 had a vasomotor disorder and 2 aircrew had neurological disorders.
The diabetic pilot was the only one to experience sexual problems, while genitourinary problems were found in the flight stewardess who experienced micturition syncope.
Analysis of the various ANS investigations led us to conclude that our aircrew presented autonomic profiles conclusive of an autonomic cause of IFI.
Vagal hyperactivity was found in 6 aircrew (66.6%), 66.6% of whom were women, vagal deficiency was found in the diabetic pilot, and 5 patients had an α peripheral sympathetic deficiency (62.5%), 80% of whom were women, responsible for low orthostatic blood pressure (BP) in 2 aircrew, and a single case of non-neurogenic orthostatic hypotension (OH) in a stewardess.
α peripheral sympathetic hyperactivity was found in 4 aircrew (44%), 75% of whom were women, in the form of postural tachycardia, without reaching postural tachycardia syndrom (POTS) values in 2 aircrew, including the diabetic pilot and a stewardess.
POTS remains a female prerogative, and was found in one female captain and one female stewardess, whose POTS is often complicated by malaise, in which case we speak of complicated POTS.
Table 2: Distribution of MEV According to Presumed Dysautonomic Etiology. G-LOC: G Induced Loss of Consciousness, OH: Orthostatic Hypotension, POTS: Postural Orthostatic Tachycardia Syndrome, CAN: Cardiac Autonomic Neuropathy
|
In flight incapacitation |
Etiology |
Numbers |
|
Percentage |
|
Perte de cognizance |
G-LOC (4Gz) + vagal hyperactivity |
2 |
7 |
78% |
|
Vasovagal syncope |
2 |
|
|
|
|
Micturition syncope |
1 |
|
|
|
|
OH |
1 |
|
|
|
|
Complicated POTS |
1 |
|
|
|
|
Access de tachycardia |
POTS |
1 |
2 |
|
|
CAN |
1 |
|
|
|
Aircrew |
FIT |
Temporarily Unfit |
Definitively Unfit |
|
|
stewardess |
0 |
4 |
1 |
|
|
Pilots |
Fighter pilot |
1 |
0 |
1 |
|
commercial pilot |
0 |
1 |
0 |
|
|
Military transport pilot |
0 |
0 |
1 |
|
The rate of permanent unfitness is 33%. The remainder are temporary unfitness, or fitness by derogation with subsequent resumption.
The notion of medical incapacity to fly refers to any physical or psychological phenomenon likely to diminish the flight performance of an aircrew. This incapacitation of the pilot is always accompanied by a threat to FS, a constant source of concern for the medical expert.
Clinical and paraclinical investigations are well codified, with the aim of finding an organic cause that could explain the malaise.
Depending on the context, this diagnostic approach may include a cardiovascular investigation: electrocardiogram (ECG), rhythmic Holter, A transthoracic echocardiogram and an exercise ECG), to rule out heart disease, a rhythm or conduction disorder, as well as a neurological investigation (electroencephalogram and brain imaging) to rule out a cerebral tumor or vascular pathology, or an epileptic disease.
Secondly, if no organic cause is found, it is advisable to look for of a predisposition to IFI, in particular by means of Ewing’s cardiovascular reactivity tests, which look for dysautonomia’s such as vagal hypertonia, OH, POTS.
These cardiovascular tests for ANS exploration were first proposed by Ewing and then detailed by Plow [2,4].
This involves continuous measurement of HR during a cycle of six deep inspirations/expirations, performed for one minute. Respiratory frequency influences the R- R space. This test is of major interest in determining vagal response. A sinus arrhythmia of respiratory origin is physiological, and depends on vagal activity: this decreases when pulmonary receptors are stimulated by stretching. The variability of the R-R space is studied by ECG recording throughout the test. The ratio of R-R in exhalation to R-R space in inspiration (minimum and maximum R-R) is studied. Pulse rate variation must be greater than 15 beats/min, and the exhalation/inspiration ratio greater than 1.2. Absence of variation in heart rate during respiratory movements indicates parasympathetic system involvement. The result is given as a percentage (maximum R-R-Minimum R-R/Minimum R- R) x100. An increase of 30% is considered normal; above 30% we speak of hyperactivity and below 30% of vagal deficiency.
This is a manual contraction performed to determine changes in BP during static effort. It involves the patient applying maximum pressure with the hand, using a dynamometer, for 15 seconds. In the normal state, muscular contraction leads to an increase in HR, which is due firstly to a withdrawal of the vagal brake, then to effort- and time-dependent sympathetic activation, and secondly to an increase in BP, which is secondary to an increase in cardiac output and peripheral resistance.
For vagal response, this test looks for a HR response 15 seconds after maximum pressure is applied with a dynamometer. Once the maximum pressure has been determined, the patient is asked to maintain a pressure 50% lower than the maximum pressure for a period of 3 minutes. This test explores the small-caliber fibers of the sympathetic efferent pathway of the reflex arc; as a rough guide, a 10% increase is considered normal; above 10% we speak of hyperactivity, and below 10% of vagal or sympathetic deficiency.
This is a simple, non-invasive quantitative test limited to studying changes in HR during the Valsalva maneuver. In this test, the patient performs a blocked exhalation after deep inspiration by blowing into a mouthpiece connected to a manometer and maintaining a pressure of 40 mm Hg for 15 seconds, followed by an abrupt cessation of effort. An ECG trace is recorded during the maneuver, and the RR ratio is calculated over three successive Valsalva sessions (ratio between the longest and shortest RR during the maneuver). This ratio must be greater than 1.20. A ratio of less than 1.10 indicates impaired ANS and arterial baroreflex. The ratio decreases with age.
This maneuver is contraindicated in cases of high blood pressure, severe hypotension or a history of stroke or retinal anomalies. It tests both the sympathetic and parasympathetic systems.
Psychic stress induces an increase in central sympathetic activity, with reduced blood flow to the extremities, tachycardia and hypertension. These responses are absent in dysautonomia, but also in some normal subjects, making the test unreliable. This test explores sympathetic efferent pathways in this test, the subject is asked to subtract the number 7 successively from 7 to zero.
α and α central sympathetic activities are expressed as variations in BP and HR respectively, before and after stimulation, according to the following formula:
BP (or HR) after stimulation - BP (or HR) before stimulation / BP (or HR) before stimulation. The result is expressed as a percentage
This involves stimulation of the sympathetic system. In normal subjects, the transition to an upright position triggers a whole series of physiological adaptation processes: large volumes of blood are displaced. This lowers venous return to the heart, causing stroke volume and BP to fall by around 40%. Baroreceptors detect these changes and transmit their signals to the cardiovascular center, which responds by stimulating sympathetic tone. Under physiological conditions, the moderate drop in aortic pressure is corrected within 30 seconds by the activation of baroreflex arcs, originating from the carotid and aortic baroreceptors, resulting in arterial vasoconstriction and tachycardia.
The patient lies on a tilting table with pedal support, and is gradually inclined up to 80° for 10 to 15 minutes. The duration can be extended to 30 to 40 minutes, depending on the pathology being investigated. parameters (HR and BP) are measured during the examination. Clinical and parametric signs of OH, POTS or syncope are sought. Pharmacological sensitization (isoprenaline, trinitrin, ) can also be performed during this test.
In this test, the subject uses his muscles to stand up. This test consists in measuring the variation in HR and BP in response to an active rise performed in less than 5 sec after a period of decubitus rest, and monitoring these parameters one minute after rising. Clinical and parametric signs of OH, POTS or syncope are sought.
These Tests can be Divided into two Categories
Tests to Study Parasympathetic Function (Vagal Response)
Tests to Study Sympathetic Function
These tests revealed a dysautonomic origin in 50% of cases. This is very similar to the results of JM Lareau’s study, in that 43% of the 65-aircrew suffering from IFI had a dysautonomic background, including 24 cases of vagal hyperactivity and 4 cases of OH, thus demonstrating the importance of the ANS in the genesis of IFI [5]
The predominance of dysautonomia IFI in stewardesses could be explained by the conditions of their work, which is mainly performed in an orthostatic position that stimulates the baroreflex, in addition to the effects of other aeronautical constraints on the ANS, which will be detailed later.
With regard to the semiology of IFI, the polymorphism observed in our study is similar to that of JM Lareau’s study, with a predominance of neurosensory manifestations [5].
However, in our study, cardiovascular manifestations rank second, which is discordant with the other study. This may be due to the dysautonomic nature of the IFI included in our study.
Thanks to the exploration of the ANS using Ewing’s tests, we were able to establish a precise autonomic profile for each aircrew suffering from IFI whose first-line etiological investigation proved negative, enabling us to diagnose ANS dysregulations including vagal hyperactivity or deficiency, α sympathetic hyperactivity and α sympathetic deficiency.
Vagal hyperactivity was found in 62.5% of aircrew, with a clear predominance of women (66.6%). In JM Lareau’s study, it was found in 37% of aircrew hospitalized for IFI [5]. This difference could be explained by the more precise exploration in our study using the Deep Breathing test, which is the gold standard for assessing vagal activity, in addition to the handgrip and orthostatic tests.
In 80% of cases, this vagal hyperactivity was associated with alpha- sympathetic deficiency responsible for low baseline and orthostatic blood pressure, with an average age of 33+/-8.94 years. This is in line with the literature, which confirms the frequency of this dysautonomia in young people, unlike sympathetic hyperactivity, which is the prerogative of the elderly, particularly diabetics and hypertensives subjects. The predominance of females is also reported in most series [2-8].
Based on the different autonomic profiles found, dysautonomic syndromes have been individualized, such as reflex and vasovagal syncope, OH, POTS and Cardiac autonomic neuropathy (CAN). It should be remembered that all these syndromes can explain the onset of IFI.
In our series, there were 9 cases of in-flight incapacitation, including 7 cases of loss of consciousness and 2 attacks of in- flight tachycardia.
Among the 7 aircrew victims of in-flight loss of consciousness, 2 G-loc at low acceleration levels (4G), 2 vasovagal syncope (VVS), 1 micturition syncope, and 1 case of syncope due to OH. The last case of syncope was related to a complicated form of POTS.
The 2 cases of fighter pilots with in-flight syncope are interesting to detail, given their severity and the importance of the aeronautical constraints to which the fighter is subjected, and which constantly solicit the ANS in turn. In high-performance aircraft, pilots undergo a cardiovascular adaptation during the initial +Gz acceleration phase, consisting of sympathetic stimulation and parasympathetic inhibition, with the aim of increasing heart rate and cardiac output. This adaptation, which is a non-immediate reaction, is characterized by a progressive decay in the event of prolonged Gz, with cessation at the end of acceleration. Consequently, in the case of ANS dysfunction, particularly that found in our pilots (vagal hyperactivity and central and peripheral α sympathetic deficiency) we can easily understand the risk of vasovagal reactions, during +Gz accelerations or when they have just stopped. Such reactions are reproducible in a stress test with a sudden stop as was the case with one of our 2 pilots, who felt uneasy when he stopped the exercise ECG test.
However, the tilt test is considered the best diagnostic tool. In JM Lareau’s study, it was positive in 58% of aircrew hospitalized for IFI, demonstrating the importance of the vagal terrain in the genesis of this malaise, and in 54 to 68% of patients presenting with syncope or presyncope, as explained in other recent studies [9].
Positive responses can be classified into three types according to the classification of VVS International Study, so that the precise mechanism can be identified:
a mixed response with falling HR and BP. Nevertheless, the limitations of the tilt-table test must also be emphasized. Although this test is useful for confirming the diagnosis of vasovagal episodes, it is not as clear that it can predict the risk of recurrence.
Finally, some authors consider other factors to be more important in predicting the risk of recurrence, including the number of episodes and psychological state [8]. Psychiatric disorders such as anxiety, mood and somatization disorders appear to increase this risk [10,11].
Indeed, in these vasovagal reactions, psychosocial aspects appear to be important. In a study of 47 aviators, the psychosocial characteristics of 24 aircrew experiencing a vasovagal episode were compared with 26 control subjects. The syncope group was found to be less psychologically flexible and to have more negative feelings about their work [12,13]. In one of our fighter pilots, psychosocial factors seem to be involved, since the psychological evaluation revealed professional conflicts, with repercussions on motivation.
With regard to vasovagal reactions in stewardesses, altitude hypobaric exposes the body’s closed cavities to expansion in a proportion ranging from around 20% between 3 and 5,000 feet, to 30% at 8,000 feet cabin pressure (2,438 meters), resulting in activation of vasovagal reflexes [14,15]. Jet lag also appears to affect ANS function. In this context, studies have shown that after a trans-meridian flight, ANS activity varied according to the disruption in circadian rhythm, with a particular increase in parasympathetic tone, requiring up to a week to return to pre- flight values [16].
In addition, aeronautical (repeated flights), physical and psychological overwork alters sympathetic-adrenergic responses, furthermore, hypoglycemia related to skipped meals, due to work rhythms, is an additional factor frequently found in our aircrew, likely to trigger vagal malaise [17].
In-flight micturition syncope, reported by one of our stewardesses, is a particular form of reflex syncope, occurring during or immediately after micturition, and can occur at any age. It is due to an abrupt failure of the ANS, with activation of the vesical receptors, resulting in a hypotensive cardiovascular response. Diagnosis is based on questioning, which reveals the prodromal symptoms classically reported in SVV. An ECG will rule out a cardiac cause, and only in case of doubt will a transthoracic echocardiogram be requested [18]. Fatigue and lack of sleep are predisposing factors found in our hostess. Patients suffering from this type of syncope should be reassured, given the low risk of recurrence.
OH syndrome, found in one of our hostesses, accounts for 6% of IFI in JM Lareau’s study. It is widely reported in the literature, and during the transition from the supine to the upright position, the ANS is sometimes unable to maintain sufficient vascular resistance [19,20]. This can lead to orthostatic syncope, as in the case of our hostess. Orthostatic hypotension is a physical finding defined by the American Autonomic Society and the American Academy of Neurology as a systolic blood pressure decrease of at least 20 mm Hg or a diastolic blood pressure decrease of at least 10 mm Hg within three minutes of standing [21]. OH, is either due to organic or functional damage to the baroreflex-vegetative arc. the ANS. The easiest way to distinguish between the two situations is to measure heart rate during the drop in blood pressure. When HR rises by more than 15 bpm, the ANS is considered to be anatomically intact, and we speak of sympathectomy OH, as was the case with our hostess. A heart rate increase of less than 15 bpm indicates damage to the ANS [22,23]. There are, however, special cases which do not obey this rule, such as diabetes, chronic alcoholism.
POTS is the chronic form of orthostatic intolerance, affecting mostly young women [24]. In our study, we reported 2 cases of POTS in two females, the first in a captain and the second in a stewardess in whom POTS was complicated by loss of consciousness. In these 2 cases, α sympathetic hyperactivity was associated with major vagal hyperactivity, as reported in the study by Benjelloun et al, vagal activity in POTS would increase to compensate for the increase in sympathetic activity [25].
POTS is defined as a rise in heart rate of more than 30 bpm or heart rate >120bpm, without OH, during the first 10 minutes of orthostatism [26]. The observed symptoms are suggestive of panic attack syndrome and have been present for more than 6 months. Clinical and paraclinical examinations are normal. It should be averted in the presence of anemia or hyperthyroidism, or after dehydration or prolonged bed rest, or in the presence of autonomic neuropathy. Its pathophysiology is highly complex. It is mainly thought to be due to a reduction in blood volume or the presence of a vasodilator in the circulation. It has also been suggested that orthostatic intolerance is caused by an anomaly in central or peripheral autonomic regulation, either due to regional sympathetic denervation of the lower limbs, responsible for blood sequestration at this level and hence primary hypovolemia, or due to hypersensitivity of the α adrenergic receptors, a state of hyperadrenergic (high levels of plasma norepinephrine). The rise in heart rate may be constant, leading to syncope with collapsed blood pressure. This is known as complicated POTS. Figure 2 shows the HR curve of our hostess during the orthostatic test [25].
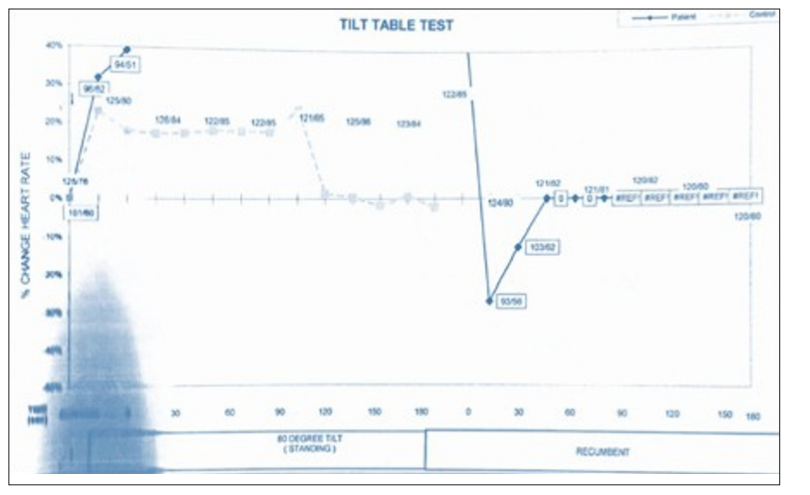
Figure 2: Example of POTS in our Hostess, HR Increases by more than 40% during Orthostatism and is maintained for at least three minutes
Once again, the activity of stewardesses, which which usually requires the orthostatic position, accentuates the symptomatology of POTS, as does aeronautical stress. In addition, exposure to hypoxia stimulates the sympathetic system, resulting in the release of adrenaline in proportion to the increase in altitude, and paradoxically exposes the patient to an increased risk of orthostatic intolerance, already present in POTS [27-31].
Cardiac autonomic neuropathy (CAN) is an abnormality of the sympathetic and parasympathetic systems, secondary to an alteration in nerve endings to the heart and blood vessels, which results in abnormal control of HR or vascular function. This frequent complication in diabetics is still underestimated compared to the other micro and macroangiopathic complications of diabetes. Men seem to be more affected than women. Risk factors that may contribute to the development of CAN include obesity, hypertension, dyslipidemia, smoking and the presence of retinopathy or peripheral neuropathy. Resting sinus tachycardia and loss of HR variation are early markers of CAN, while OH is later.
Investigation of the ANS often reveals a vagal deficiency with sympathetic hyperactivity, as in the case of our diabetic transport pilot who presented with IFI in the form of a tachycardic episode, and in whom the baseline HR was relatively high on clinical examination. Elevated HR in diabetic subjects is generally attributed to parasympathetic dysfunction [32].
In diabetic patients with CAN, a decrease in parasympathetic tone occurs during the night, and the nocturnal predominance of sympathetic activity may predispose to cardiovascular events. Furthermore, sympathetic hyperactivity maintains chronic hyperglycemia by increasing hepatic glucose production and decreasing skeletal muscle glucose utilization [33].
Fitness is managed on a case-by-case basis, depending on the dysautonomic pathology, the aircrew specialty and the compatibility of the treatment with aeronautical activity. Sufficient time must be allowed to elapse, with monitoring by autonomic tests, in order to prove the efficacy of the treatment and its tolerance. Three of our pilots have been considered for permanent unfitness. The first case involved a fighter pilot with hyper vagotonia and sympathetic deficiency, a profile incompatible with flying high-performance aircraft, which led to a decision to disqualify him from flying fast aircraft. Given the pilot’s demotivation, a multi-pilot derogation for transport was not an option.
The second case is that of a transport pilot with diabetes, who was already fit to fly by derogation with a temporary restriction due to his diabetes. The discovery of CAN, a serious complication of the diabetes, in this pilot who was nearing retirement age and had lost his motivation, led to the declaration of definitive unfitness. The stewardess diagnosed with complicated POTS represents the third case of permanent unfitness. Given the lack of clinical improvement and orthostatic testing, and the recurrence of syncope despite treatment, fludrocortisone was introduced. The incompatibility of the latter with THE FS was behind the final decision of unfitness.
Our study reveals the importance of exploring the ANS in the case of any IFI for which the etiological investigation finds no organic cause that could explain the malaise. Consequently, the flight surgeon must be made aware of the high frequency of these dysautonomic disorders in aircrew subjected to the various aeronautical stresses involving the ANS. The aim should be to look for functional signs of dysautonomia, and even to perform a few tests that may point to an ANS anomaly, such as OH or POTS in the active orthostatic test performed during the consultation. Additionally, our study also raises the issue of the incompatibility of certain treatments for these dysautonomia’s with FS. In such cases, the aircrew fitness to fly is at stake.
The authors declare no conflict of interest
All authors have contributed to, read and approved the submitted version of this article
