Author(s): Noha Amail, Lazhar Hanaa*, Khaoula Lakhdar, Oumaima Fakir, Aziz Slaoui and Aziz Baydada
Longitudinal vaginal septum is subsequent embryologically to a lack of resorption of the lower part of the Mullerian canals. Other genital malformations can be associated in varying proportions. In fact, there are three types of longitudinal vaginal septum: isolated longitudinal vaginal septum, vaginal septum associated with a septate uterus and vaginal septum associated with two hemi-uterus [1].
This septum may present clinically as a difficulty in inserting tampons, persistent bleeding despite the presence of a tampon, or dyspareunia. On the other hand, it may be asymptomatic [1]. The treatment consists of a complete resection of the septum.
We hereby present the uncommon case of a 21 years old primigravidae that consulted our obstetrics emergency department for onset uterine contractions at 38 weeks of gestation. She had no family or personal history of genitourinary malformations. Her menarche was at 10 years old. However, she reports a few episodes of intermittent dyspareunia during sexual intercourse. Her pregnancy was conceived naturally and she had no follow-up. Her general assessment showed an acute labor and no sign of distress. Her physical examination revealed a stable patient with a uterine height of 30cm presenting regular uterine contractions of normal intensity. Fetal heart sound rate was regular and reactive ranging from 120 to 160 bpm. Vaginal examination found an 80% shortened cervix, dilated to 3 cm with cephalic presentation and intact membranes. Through bimanual examination, an elastic structure was felt -painlessly- approximatively 3 cm above the vaginal introitus going from the anterior to the posterior vaginal wall separating the vaginal canal in two. A more detailed examination was made by inserting a Collins speculum, revealing a complete longitudinal non-obstructing vaginal septum in the distal third of the vagina with one uterine cervix. Pelvic examination noticed no other abnormalities.
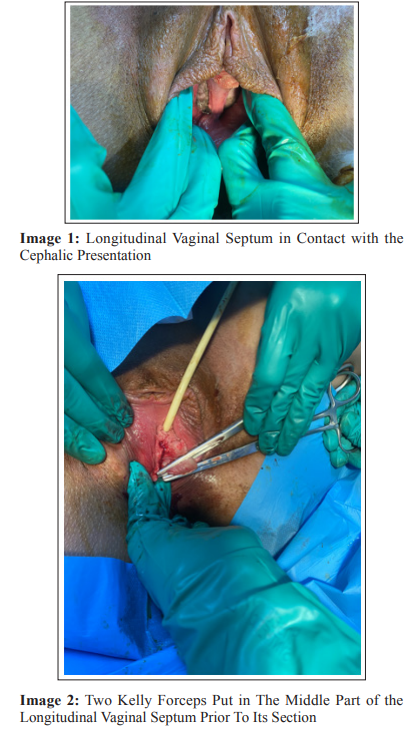
An obstetric ultrasound was performed and showed an evolving pregnancy in cephalic presentation, an amniotic fluid of normal quantity, a fundal placenta with an estimated fetal weight of 3000g. Vaginal delivery was accepted under epidural after vaginal septum’s transection. Therefore, the parturient was transferred to the delivery room. We opted for a classical surgical approach by excising with scissors after the application of 2 Kelly forceps to prevent blood loss, after which the edges were sutured for hemostasis with 3-0 absorbable sutures.
Labor progressed satisfactorily allowing the natural delivery of a female baby weighing 3050gr with an Apgar score of 9/10 with no apparent congenital malformation. After delivery, we performed a complete resection of the two upper and lower edges of the septum. Postpartum follow-up was uncomplicated with a complete restoration of the vaginal anatomy. Six months after delivery, the patient underwent a three-dimensional ultrasound, a hysterosalpingography, and hysteroscopy to make sure there was no other congenital abnormalities associated with the vaginal septum. Moreover, dyspareunia was relieved and the quality of her sexual life was better.
Abnormal development of the müllerian ducts occurs in a variety of forms. The incidence ranges from 2-3% in fertile women [2]. In fact, the complex development of the genital tract during embryogenesis involves a series of events including cell differentiation, migration, fusion, and canalization[3]. Any failure in this process may generate a congenital abnormality
The distal third of the vagina arises from the urogenital sinus while the proximal two-thirds originate from the fusion of the Mullerian ducts [4]. The sinovaginal bulbs proliferate at the caudal end of the uterovaginal canal to become a solid vaginal plate. Then, the lumen of the lower vagina is formed via apoptosis of the central cells in this vaginal plate, extending in a cephalic direction. Complete canalization occurs by 20 weeks of intrauterine life [5]. In recent decades, advances in imaging techniques have facilitated diagnosis of Mullerian duct anomalies, the incidence of which is estimated at 0.001 to 10% [6]. The longitudinal vaginal septum is typically associated with uterine anomalies such as a septate uterus or uterus didelphys [7].
It may be complete or partial. Clinically, the septum may present as a difficulty in inserting tampons, persistent bleeding despite the presence of a tampon, or dyspareunia. On the other hand, it may be asymptomatic [1]. The difficulty of the diagnosis of this anomaly is due to the lack of symptoms. On the contrary due to its association with uterine abnormalities, it often leads to infertility or pregnancy loss. In our case, the diagnosis was made during labor of a primigravidae who was complaining of dyspareunia since the onset of her sexual life. Subsequently to any vaginal abnormality, a genitourinary investigation is mandatory. Thanks to its ubiquity, the ultrasound deserves its place as the first and the most common imaging tool. However, the MRI is still the gold standard [8].
Treatment involves complete resection of the septum which may be performed during vaginal delivery, thus avoiding a cesarean section, as performed in our case. Ideally, resection should be performed prior to pregnancy [1]. The management requires, during delivery, two steps. The first step is the ligature and section of the septum when the presentation is about to be in contact with it and start pushing the tissue and the second step is the resection of the septum after the delivery [9]. An examination 2 or 3 weeks after delivery should be part of the patient’s follow up so as to assess the anatomical structure of the vagina.
Longitudinal vaginal septum is a rare condition. Its discovery during delivery should not be an absolute indication of caesarean. The ligature and section of the septum when the presentation came on its contact can avoid unnecessary caesarean section and reduce patient’s morbidity. Its prompt diagnosis during early teen years enables concise urogenital investigations allowing adequate treatment before the onset of sexual intercourse and pregnancy.
N/A.
N/A.
