Author(s): Christian Perez Calvo*, Michel Perez Marrugo, Emerson Javier García Ballesteros, Alejandro Alberto Nuñez Ospino, Luis Saray Ricardo, Gabriel Padilla Vega, Carlos José Brito Jacome, José María Mejía Barrera, Julio Contreras Pasimino, Jhohanna María Parra Pizarro, Felipe Herrera Lozano
Diabetic kidney disease is one of the microvascular complications with the greatest impact on morbidity and mortality in patients with diabetes. Previously thought to be a linear series of events consisting of ultrafiltration, glomerular hypertension, albuminuria, and successive decreases in GFR, it is now known to be affected by multiple metabolic and hemodynamic pathophysiological mechanisms, leading to cell signaling pathways, oxidative stress, dysregulated autophagy, triggering structural damage and functional alterations leading to disease. There are also recognized risk factors for the disease that trigger pathophysiological mechanisms that contribute to its development, such as obesity, smoking, poor metabolic control, arterial hypertension, ethnicity, among others. Although current therapies have not completely halted the development of the disease, current efforts are focused on developing new therapies that can positively influence its onset and progression, with both SGLTi and AR-GLP1 playing a leading role, improving cardiovascular and renal outcomes, independently of their effect on the control of hyperglycemia, which is why they are currently a fundamental pillar of management. Finerenone, a mineralocorticoid receptor antagonist, is another current therapy that has been shown to have an impact on cardiovascular and renal outcomes, playing a complementary role to ACEI and ARB II in the management of albuminuria.
Diabetic kidney disease (DKD) is a microvascular complication that occurs in type 1 and type 2 diabetes, which increases morbidity and mortality compared to those who do not develop it, often progressing to end-stage renal disease (ESRD), with the need for renal replacement therapy [1].
Diabetic Nephropathy (DN) was traditionally considered as a series of sequential stages, starting with hyperfiltration and glomerular hypertrophy, followed by albuminuria, leading to deterioration of renal function. Currently, DN refers to the microangiopathic lesion produced by diabetes mellitus, with involvement mainly of the glomerulus, characterized by persistent proteinuria, arterial hypertension and progressive worsening of the glomerular filtration rate (GFR). It is recognized that a notable group of patients develop deterioration of GFR without going through intermediate stages, so the current paradigm defining diabetic kidney disease is deterioration of renal function. The term currently in general use is diabetic kidney disease, since it is a broader definition that encompasses diabetic patients with renal involvement [2, 3].
Tight glycemic control, blood pressure (BP) treatment, cardiovascular risk reduction and nephroprotective measures targeting the renin angiotensin aldosterone system (RAAS) can delay the progression and development of diabetic kidney disease [2].
The International Diabetes Federation estimated a global prevalence of diabetes in adults aged 20-79 years in 2021 of 10.5%, by 2030 it projects an increase to 11.3% and by 2040 up to 12.2%. An estimated 240 million people worldwide have undiagnosed diabetes, meaning that nearly one in two adults with diabetes does not know they have it [4].
DRE is one of the microvascular complications with the greatest impact on the prognosis of patients with diabetes mellitus and the main cause of end-stage renal disease. The incidence of DRE has doubled in the last decade due to the increase in cases of type 2 diabetes. It is currently estimated that about 25-35% of those diagnosed with type 2 diabetes already have microvascular complications [5].
All-cause mortality in persons with ESRD is approximately 30 times higher than in diabetic patients without ESRD; the vast majority of patients with ESRD die from cardiovascular disease before developing end-stage renal disease [5].
The risk factors for DRE are conceptually classified into susceptibility, initiation and progression factors (Table 1), among which hyperglycemia and hypertension stand out [6, 7].
In normoalbuminuric patients with type 1 diabetes, poor glycemic control has been Shown to be an independent predictor of progression to the development of albuminuria and/or ESRD [6-8]. Inadequate blood pressure control (SBP >140) in patients with type 2 diabetes has been widely associated with a higher risk of mortality and of developing ESRD [9].
| Risk Factors for Diabetic Kidney Disease | |||
|---|---|---|---|
| Demographic | Susceptibility | Initiation | Progression |
| Older age | + | ||
| Sex (Man) | + | ||
| Race/ethnicity (black, American Indian, Hispanic, Asian/Pacific Islanders) | + | + | |
| Hereditary | |||
| Family history of DKD | + | ||
| Genetic kidney disease | + | ||
| Systemic conditions | |||
| Hyperglycemia | + | + | + |
| Obesity | + | + | + |
| Hypertension | + | + | |
| Kidney injuries | |||
| Acute kidney injury | + | + | |
| Toxins | + | ||
| Smoking | + | + | |
| Dietary factors | |||
| High protein intake | + | + | |
Figure 1: Review on pathophysiology of DKD.

DRE has traditionally been explained as the result of the sum and relationship between hemodynamic and metabolic factors; however, it is currently known that a complex network of events that determine renal damage are involved in its development, including: susceptibility factors (gender, race, age, family history and genetics), progression factors (diet, obesity, arterial hypertension) and the initiating element, which is hyperglycemia [10].
Among the hemodynamic factors are increased intraglomerular pressure and hyperfiltration, both of which occur in the early stages of diabetes and contribute to the development and progression of DRE, Ultrafiltration may be explained in part by unregulated tubuloglomerular feedback. In hyperglycemia, hyperfiltration of glucose increases renal tubular reabsorption of glucose and sodium in the proximal tubule, resulting in a reduced distribution of sodium to the distal tubular macula densa, leading to a significant decrease in the resistance of afferent arterioles and consequently to increased pressure in the glomerulus [11].
The increase in glomerular pressure produces mechanical stress on the capillary wall, which causes glomerulosclerosis and destruction of peritubular capillaries, and also increases the filtration of proteins into the tubular lumen, which causes the production of proinflammatory and profibrotic factors that lead to renal damage [11].
Hyperglycemia activates metabolic pathways that generate reactive oxygen species (ROS), such as the polyol pathway, the hexosamine pathway, the protein kinase C (PKC) pathway and the advanced glycation end products (AGE) pathway. ROS oxidize important macromolecules, including proteins, lipids and nucleic acids, which ultimately lead to tissue damage [11, 12].
In diabetes, mitochondrial function is altered which also leads to increased levels of ROS by positive feedback from prooxidant enzymes such as nicotinamide adenine dinucleotide phosphate (NADPH). Such accumulation of ROS and superoxides is considered the main trigger for the events that lead to complications in diabetes mellitus including DRE [13].
On the other hand, insulin resistance, elevated blood glucose levels and increased blood insulin levels independently cause endothelial dysfunction by promoting several intracellular mechanisms, such as increased production of reactive oxygen species (ROS), protein kinase C (PKC) and advanced glycation end product (AGE) inducing proinflammatory signaling [14].
Interactions of mediators produced by endothelial cells are disrupted and tend to become imbalanced, among these mediators, endothelin-1 (ET-1) is the most potent vasoactive peptide produced by endothelial cells to regulate vascular homeostasis. In endothelial cells, compensatory hyperinsulinemia increases ET-1 secretion, leading to vasoconstriction and vascular dysfunction. In the kidney, endothelin a receptor activation is associated in addition to vasoconstriction with podocyte damage, oxidative stress, inflammation and fibrosis [15, 16].
Renal hypoxia and inflammation are also essential factors in the development of DRE, it is known that hypoxia is the result of an inadequate balance between oxygen requirements and oxygen supply; in diabetes and hyperglycemia the energy expenditureof the tubular cells is increased, which leads to an increase in the activity of the sodium-glucose cotransporter and glomerular hyperfiltration [17].
Although there is an increase in oxygen consumption, oxygen supply is diminished in RDE due to multifactorial causes, including loss of peritubular capillaries and interstitial fibrosis [18]. Studies based on magnetic resonance imaging with oxygen level-dependent contrast imaging in animal models have shown that low oxygenation at the level of the renal cortex was an independent predictor of decreased renal function [19].
Inflammation plays a determining role in the development of DRE by various pathophysiological mechanisms; the independent relationship between C-reactive protein (CRP) and albuminuria in diabetic patients has been described, and the role of multiple inflammatory cytokines as triggers of renal damage in DRE stands out in this process [20].
IL-1 is associated with increased expression and uptake of chemotactic factors and adhesins in endothelial and mesangial cells, in addition to dysregulation of hyaluronic acid synthesis in the tubular epithelium and increased endothelial permeability, as well as intraglomerular hemodynamic alterations. IL-6 is associated with changes in endothelial permeability, mesangial cell proliferation and increased fibronectin expression. Renal IL-6 expression correlates directly with the severity and structural changes of renal hypertrophy and glomerular injury in RDE [20, 21].
As for IL-18, this molecule is associated with an increase in albuminuria and changes in this parameter during renal disease, suggesting that elevated levels of this cytokine may be a predictor of early renal dysfunction in normoalbuminuric diabetic patients [20, 21].
Among the inflammatory mediators, TNFa also stands out; this molecule has biological activities that may be related to renal injury in diabetic patients: direct cytotoxicity to renal cells, induction of apoptosis, and alteration of intrarenal hemodynamics, and increase in endothelial permeability or induction of oxidative stress. In experimental models of DM, renal TNFa levels are elevated, which is associated with renal hypertrophy and hyperfiltration, initial alterations in the development of RDE [22, 23].
Finally, the nuclear transcription factor kappa B (NF-Kb) has been identified as a key factor in the inflammatory pathways involved in ERD. This factor is inactivated in resident cells; however, before stimuli triggered by hyperglycemia, AGEs, mechanical stress, proteinuria, angiotensin II, it is activated; once activated, it plays a central role in the activation and recruitment of cytokines, chemokines and adhesion molecules [24, 25].
The activation and hyperactivity of the renin angiotensin aldosterone system (RAAS) also play a key role in the deterioration of RDD, since there are multiple clinical trials and animal models where it has been demonstrated that the inhibition of this system delays the progression of renal damage in RDD, it is also known that Angiotensin II and transforming growth factor (TFG-B1) promote the development of renal fibrosis and renal tubular atrophy, induce chronic hypoxemia and promote microcirculation impairment [26, 27]. Aldosterone is also believed to play an important role in the pathophysiology of RDE by regulating gene expression and other mechanisms, including up-regulation of pro-sclerotic growth factors such as plasminogen activator inhibitor-1 (PAI-1) and TGF-B, and promotes macrophage infiltration and subsequent renal fibrosis [27, 28].
Recent studies have shown that dysregulated autophagy also plays an important pathogenic role in DRE. Autophagy is the cellular degradation of macromolecules and organelles to preserve cellular homeostasis. Autophagy has two main physiological functions; one is to recycle intracellular resources according to nutrient requirements, another is the removal of damaged proteins and organelles under various stress conditions [29, 30]. The importance of autophagy in the pathogenesis of ERD was highlighted in a study using podocyte-specific autophagy-deficient mice, which showed podocyte depletion and massive proteinuria after a highfat diet [31].
Recently, genetics and epigenetics have attracted great interest since recent evidence shows that they play a relevant role in the pathophysiology of RDD. Epigenetic modifications include DNA methylation, non-coding RNAs, histone post-translational modifications, which have been shown to be triggered by hyperglycemia, hypoxia, inflammation and mediators such as cytokines [32].
Such modifications cause the individual's cells to acquire metabolic memory such that even if the patient obtains adequate control with medical interventions such as proper diet, weight and glycemic control with drugs or insulin therapy, many patients continue to experience numerous complications associated with DRE, suggesting the existence of a "memory" of previous exposure to hyperglycemia in target cells, leading to the persistence of its detrimental effects long after glycemic control has been established. Therefore, one of the current targets for approach and management is aimed at the development of epigenetic markers and modification therapies [33].
Diagnosis requires a history of confirmed diabetes and establishing the presence of renal disease, which is based on two parameters: GFR and albuminuria [34, 35].
Classically the standard test to establish albuminuria as a marker of renal damage has been the measurement of 24-hour urinary albumin excretion, however, currently the Albumin - Creatinuria ratio in a random urine sample is more frequently used, and it is established that the significant range is 30mg/g or higher, This value should be checked in at least 2 of 3 samples in a period of time of 3 to 6 months, since physiological conditions such as exercise and inadequate hydration, or pathological conditions such as urinary tract infections and congestive heart failure could temporarily alter these values, resulting in diagnostic inaccuracies [34, 36, 37].
Screening for albuminuria should begin at the time of diagnosis in type II diabetics and is recommended at 5 years in patients with type I diabetes mellitus, with annual measurements [38]. GFR is the other parameter to establish renal damage, which should be calculated with validated formulas from the serum creatinine level, being the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) group equation the currently recommended one, GFR levels persistently lower than 60ml/ min/1.73m2 are considered significant, for which two GFRmeasurements with a time interval of at least 3 months are required [38, 39].

Figure 2: Diagnostic Algorithm and Screening for Diabetic Kidney Disease
Treatment aims to avoid the complications associated with DRE, decreasing disease progression and cardiovascular risk (CVR), which includes adequate control of glycemia, blood pressure, CVR and RAAS blockade [2].
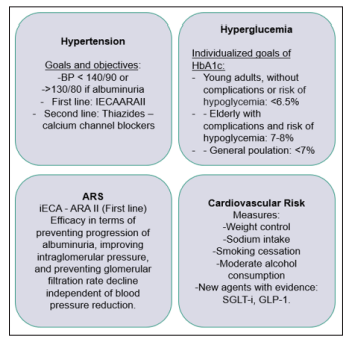
Figure 3: Essential Aspects in the Treatment of Diabetic Kidney Disease
Recently the KDIGO guidelines recommend a holistic approach that begins with the promotion of healthy lifestyles, including a healthy diet, physical activity, smoking cessation and weight control [40].
Tobacco use remains one of the leading causes of death worldwide and a known risk factor for developing CKD. Recent studies also highlight the link between passive smoking and the development of the disease; cessation of tobacco use should be recommended to all patients with CKD, avoidance of passive exposure to tobacco smoke is another advisable intervention in these patients [40, 41].
Regular exercise routines improve glycemic homeostasis, attenuate oxidative stress, optimize endothelial function and modulate inflammation and the RAAS. They have been considered a key strategy in achieving metabolic control goals and preventing complications associated with diabetes mellitus, improving patients' quality of life as well as having the potential to prevent and attenuate the development of DRD [42]. In general, regular exercise routines of moderate intensity, lasting at least 150 minutes/ week, avoiding inactivity for 2 consecutive days, should ideally contain both aerobic and resistance exercises in adult patients with type 2 diabetes [43].
The dietary changes in DRE recommended by the Nutrition kidney foundation- KDOQI (NKF-KDOQI) comprise a caloric intake of 30-35 Kcal/kg/day, giving preponderance to foods such as whole grains, fibers, fruits, vegetables, and avoiding the intake of refined sugars. They recommend a sodium intake of less than 1.5-2.3 g/day, the optimal amount of fat intake is not yet completely clear in DRE, however, it has been recommended to reduce the consumption of trans fats and saturated fatty acids, in the latter the guideline is < 7% of total daily calories, it has been shown that the consumption of polyunsaturated and monounsaturated fatty acids would have a protective effect in attenuating inflammation and endothelial dysfunction and would improve blood pressure and lipid control. Regarding protein intake in RDD, the recommendation has been to establish the intake according to the degree of renal compromise of the patients; in general, it is recommended in patients with Grade I-IV renal disease targets of 0.8/kg/day; on the contrary, in those patients on ESRD managed with renal replacement therapy, intakes >1.2g/kg/day are considered appropriate [44].
Obesity is a risk factor for multiple health conditions including hypertension, cardiovascular disease, obstructive sleep apnea and osteoarthritis, classically the body mass index (BMI) has been the measure used to measure this condition, however recent evidence suggests that the accumulation of fat in the waist or central obesity would also behave as a risk factor regardless of the BMI value. It is known that in obesity there are changes in renal structure and physiology, within the structural ones we find glomerulomegaly, mesangial expansion, sclerosis and abnormalities in podocytes, even a specific form of focal segmental glomerulosclerosis, within the functional ones there are hyperfiltration and proteinuria. Given that both RDE and obesity share characteristics in terms of anatomical and physiological alterations, it is considered that their association could have additive effects. Currently, all patients with obesity and RDD would be recommended to lose weight, especially those in non-advanced grades of disease (I-III) [45, 46].
In the patient with RDE, glycemic control plays a key role in preventing the establishment of the disease. The Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) trial showed that intensive glucose control can reduce the development of microalbuminuria and macroalbuminuria [47].
The American Diabetes Association (ADA) suggests individualizing
glycemic control goals according to the patient's profile according
to age, comorbidities and life expectancy, suggesting stricter
control expectations (HbA-1c < 6.5%) in the young patientwithout comorbidities and with good life expectancy, in contrast
looser goals (HbA-1c < 8%) should be considered in the elderly
patient with long-standing disease, macro and microvascular
complications and shorter life expectancy [48-50].
The KDIGO management guidelines suggest as a goal for diabetic
patients an HbA-1c lower than 7% with the aim of reducing and
delaying the appearance of microvascular complications; however,
they clarify that in patients at high risk of hypoglycemia, this goal
should not be so strict, accepting values above 7% but lower than
8% [39].
The current first-line pharmacological therapy in DKA in type 2 diabetic patients consists of metformin in association with a SGLT2i (sodium glucose cotransporter 2 inhibitors), provided that there is no contraindication for the administration of these drugs, since they have an impact on metabolic control as well as on renal and cardiovascular outcomes, the addition and selection of other hypoglycemic agents when metabolic control goals are not achieved, should be established according to multiple factors such as local availability of the drugs, associated costs, patient preference, comorbidities, GFR levels, with preference being given to AR-GLP1 [40].
Metformin is an oral hypoglycemic agent belonging to the biguanide group, considered a first-line agent in patients with type 2 diabetes, which has experimental studies that have demonstrated attenuation of ESRD by intervening in inflammatory mechanisms, oxidative stress and fibrosis. In clinical trials the use of metformin has been associated with decreased mortality, cardiovascular disease and progression to ESRD, however, its use should be monitored and established with caution due to the increased risk of lactic acidosis [51]. In general, the use of metformin is not recommended in patients with advanced CKD, because an increase in mortality has been observed in these patients; currently, its use is recommended in type 2 diabetic patients with GFR ≥30ml/ min/1.73 m 2, adjusting the dose according to renal function, being together with SGLT-2i the first-line pharmacological therapy [51-53].
SGLT-2i prevent the reabsorption of filtered glucose at the renal tubular level, which triggers glycosuria and lowers glycemia levels. They provide nephroprotective effects and decrease CVR in patients with DRE independently of their hypoglycemic effect [54]. The mechanism by which they produce this effect is still not entirely clear. The main hypothesis focuses on urinary sodium excretion caused by inhibition of sodium and glucose reabsorption in the proximal tubule. Increasing the concentration of sodium in the macula densa, activating the tubuloglomerular feedback that would lead to vasoconstriction of the afferent arterioles and reduction of the intraglomerular pressure [55, 56].
Regarding the adverse effects associated with SGLT-2i therapy, the most frequent are infections of the urogenital tract, being genital fungal infection the most frequent, especially in early phases of treatment, urinary infections are less usual, with even less frequency, normo-glycemic ketoacidosis can occur, educating the patient to avoid ketogenic diets, suspending the use during acute illness, or prior to surgery could reduce the associated risks [57, 58].
In the CREDENCE study, which compared canaglifozin vs. placebo in 4401 albuminuric patients with type 2 diabetes and renal disease, included patients with GFR > 30ml/min/ 1.73m2, and mean albumin/creatinuria ratio of 927mg/g. Canaglifozin evidenced a 34% decrease in the composite risk of doubling baseline serum creatinine, end-stage renal disease or renal death (HR 0.66 (0.53-0.81); p < 0.001). In addition, canaglifozin reduced three major adverse cardiovascular outcomes (3p-MACE) by 20% (HR 0.80 (0.67-0.95); p < 0.01) and hHF by 39% (HR 0.61 (0.47-90.8); p < 0.001) [59].
The DAPA-CKD study included patients with non-diabetic CKD, in patients with GFR 25-75ml/min/1.73 m2, and albuminuria, dapagliflozin demonstrated a 44% reduction in the composite renal outcome, doubling of baseline serum creatinine levels, ESRD, or renal mortality (HR 0.56 (0.45-0.68); p < 0.001) [60].
A meta-analysis confirms the favorable effects of SGLT2i on the composite renal outcome of doubling of baseline serum creatinine (40% decrease in GFR), initiation of renal replacement therapy (RR 0.63 (0.56- 0.71) or death from renal causes even in the presence of cardiovascular disease or multiple risk factors (RR 0.67 (0.59-0.76) [61].
Based on these results, the use of canaglifozin, empaglifozin and dapagliflozin is currently endorsed as cardiovascular risk prevention and nephroprotective agents in the context of diabetic kidney disease, recommending their initiation in type II diabetic patients with GFR>20ml/min /1.73 m2 and they have been suggested as first-line therapy in the KDIGO 2022 guidelines [40, 62].
They are an incretin hormone that stimulates insulin secretion in response to food intake and their analogs are used to treat type 2 diabetes [63, 64].
They are among the agents with the potential to prevent RDD, however not all those belonging to their group have demonstrated this benefit, the incretin mimetic analogues of exendin-4 such as exenatide/lixisenatide have not shown favorable results in cardiovascular outcomes whereas human GLP1-RAs such as liraglutide, dulaglutide and semaglutide have shown benefits [65-67].
In the LEADER and SUSTAIN-6 trials, treatment with liraglutide and semaglutide respectively was associated with a lower rate of major cardiovascular events or death [67-68]. In the REWIND trial treatment with dulaglutide vs placebo in 9901 participants where only 31% of participants had previously established cardiovascular disease, dulaglutide showed a reduction in 3p-MACE by approximately 12%, regardless of pre-existing atherosclerotic cardiovascular disease. A meta-analysis of seven large clinical trials of AR-GLP1 with 56 004 patients showed a 12% reduction in 3p-MACE. Composite renal outcomes were reduced by 17% for all AR-GLP1, mainly due to a reduction in macroalbuminuria [66, 69].
The cardiovascular and renal benefits provided by AR-GLP1 drugs may be related to their direct effects on blood pressure, glucose and body weight; they also ameliorate endothelial dysfunction and inflammation. Initially, they may cause a fall in GFR, which usually plateaus.
Its use is currently recommended in patients with type 2 diabetes who do not achieve glycemic control goals or persist with albuminuria despite management with first-line therapy (Metformin + SLGTi) or as a substitute in the event that the use of such therapies is not available or is contraindicated. The use of long-acting drugs is advised, starting with low doses, gradually increasing the dose in order to avoid gastrointestinal intolerance; the combination with dipeptidyl peptidase 4 (iDPP-4) inhibitors should be avoided [40, 70].
BP control in individuals with DRE has been shown to be
fundamental in delaying disease progression and decreasing
cardiovascular mortality. In the UK Prospective Diabetes Study
(UKPDS), a decrease in the risk of developing microvascular
complications of up to 37% was observed in patients who were
treated with a blood pressure goal of < 150/85 mmHg compared
to those who were treated with a target of < 180/105mmHg, in
addition, for every 10mmHg increase, a 15% increase in the
risk of developing Grade 3 chronic kidney disease (CKD) was
observed, evidenced either by the establishment of albuminuria
or a doubling of serum creatinine levels [62, 71].
Blood pressure targets have been controversial over time, The
Systolic Blood Pressure Intervention Trial (SPRINT) study in
2015 demonstrated that, in patients at high cardiovascular risk, a
decrease in systolic blood pressure (SBP) levels < 120 vs < 140,
was associated with improvement in cardiovascular and all-cause
mortality however these results could not be extrapolated to the
diabetic population as this population was excluded from the
study [72].
The ACCORD-Blood pressure study set out to investigate the
effect of tight BP control on cardiovascular outcomes particularly
in diabetic patients at high risk of cardiovascular disease.
The results showed that lower BP targets (systolic blood pressure
<120 vs <140) were associated with a lower risk of proteinuria
progression and stroke during 5-year follow-up, but without benefit
for combined fatal and nonfatal cardiovascular events. Serious
adverse events due to antihypertensive therapy were more frequent
in the antihypertensive group (3.3% vs 1.3%) [73].
Initial treatment of hypertension in patients with diabetes should
include lifestyle changes, including dietary sodium restriction
(less than 2300 mg per day), weight loss if overweight or obese,
increased physical activity, moderation of alcohol consumption,
and smoking cessation [74].
Currently the JNC 8 (Eighth Joint National Committee) and the
KDOQI guidelines recommend BP goals < 140/90 in diabetic
patients regardless of the presence of CKD, as long as there is no
proteinuria; in the presence of proteinuria this parameter becomes
stricter, the goal being < 130/80 [75].
The agents of choice for blood pressure control in patients
with RDE are angiotensin-converting enzyme inhibitors (ACE
inhibitors) and angiotensin II receptor antagonists (ARA II) [76,
77].Thiazide diuretics and calcium antagonists appear as secondline agents in case BP goals are not achieved with ACEI or ARA II,
since they seem to show cardioprotective effects, but do not seem
to have the same degree of benefit on the progression of DRE [78].
RAAS blockade is an essential strategy for the management of
RDE. The benefit of RAAS blockade in RDE is independent of
its effect on BP, probably due to a greater extent to a reduction in
intraglomerular pressure and the resulting impaired ultrafiltration
and albuminuria. Because reduced albuminuria is associated with
slower progression of DRE and better cardiovascular outcomes,
control of albuminuria is an important goal of DRE treatment.
In addition, RAAS inhibitors ameliorate angiotensin-induced
oxidative stress, inflammation, and fibrosis [72, 79].
ACEI and ARA II are the agents with the strongest evidence and
recommendation for use. Multiple randomized clinical trials with
ACEI and ARA II have demonstrated benefit in reducing the risk
of doubling of serum creatinine and the composite outcomes of
mortality and ESRD [80-82].
The Diabetes Control and Complications Trial Research Group (DCCT) study showed that captopril, independent of its effect on BP, reduced the risk of doubling serum creatinine levels by 48% over 3 years in individuals with type 1 DM and high levels of albuminuria [80].
In the RENAAL (losartan) and IDNT (irbesartan) studies, it was
shown that independently of their effect on BP, the use of these
ARA II showed a significant reduction in the composite outcome of
doubling of baseline serum creatinine, mortality or renal failure by
16% and 20%, respectively, over approximately 3 years [81, 83].
The combined use of ACEI+ARA II has not been recommended
since studies such as ONTARGET (Telmisartan + Ramipril) have
shown that, although they produce lower BP and albuminuria
levels, they do not produce additional long-term benefit compared
to monotherapy and, in contrast, significantly increase the risk of
associated adverse events such as hyperkalemia and hypotension
[84].
Mineralocorticoid receptor antagonists (MRAs) decrease albuminuria, however, they lack evidence regarding the prevention of the development of ESRD, their most common adverse effects such as hyperkalemia have been prevented in long-term studies on ERD, strategies for clinical trials include the use of potassium chelators, aldosterone synthase inhibitors and non-steroidal mineralocorticoid receptor antagonist [85].
Among the promising therapies we found a non-steroidal ARM called Finerenone, the only one in its class that has shown cardiovascular and renal benefits in two pivotal studies, especially caution should be taken given the risk of developing hyperkalemia with this drug, however in case of occurrence it could be managed with 72-hour pauses of the medication given its short half-life of action and in case of not improving with this measure, other strategies should be established [86].
In the FIDELIO-DKD (Finerenone in reducing kidney failure and disease progression in diabetic kidney disease) study has shown promising results, Finerenone achieved the primary endpoint (renal failure, a sustained decrease of at least 40% in GFR from baseline or death from renal causes) in 17.8% of patients compared to 21.1% on placebo (HR: 0.82, CI: 073 to 0.93, p = 0.001) [87, 88].
In the FIGARO-DKD study, finerenone therapy improved cardiovascular outcomes compared to placebo in patients with type 2 diabetes who had CKD Grade 2-4 with moderately elevated albuminuria or CKD Grade 1 and 2 with severely elevated albuminuria. Therefore, finerenone may represent an importanttherapeutic option in CKD, and its use is currently recommended in the context of persistent albuminuria despite the use of an ACEI or ARA II, in patients with normal potassium [40, 89].
DKA is a microvascular complication of diabetes mellitus that leads to increased cardiovascular risk with great impact on the morbimortality of diabetic patients; its prevalence is on the rise due to the progressive increase in cases of diabetes mellitus, mainly type 2, Currently, DRD is recognized as a disease with dynamic and diverse pathophysiological mechanisms that occur simultaneously and not always in a linear fashion, where the markers that define the presence of the disease are GFR and albuminuria; however, it is expected that in the future, with a better understanding of the pathophysiology, even earlier markers will be developed. Current treatments can slow down the course of the disease, but not stop it completely. Establishing individualized guidelines according to the patient's profile and comorbidities, starting with lifestyle modifications, establishing recommended first-line therapies up to interventions guided to specific objectives, impacting CVR, ARAS, glycemic control and BP, has been the most recommended approach. Therapy with an ACEI or ARB continues to be the gold standard in terms of RAAS axis blockade. Cardiovascular risk reduction is one of the most important goals in these patients, and the most relevant innovative therapies are SGLT2i and AR-GLP1, two promising groups of drugs, being agents with a very good safety profile, which in addition to contributing to the goals of glycemic control, have been shown to have a favorable impact in the available studies on both cardiovascular and renal outcomes. Finerenone, a non-steroidal ARM, is another therapeutic option that has shown evidence in both renal and cardiovascular outcomes. Further studies are needed to better understand the pathophysiology, which will allow us to establish novel therapeutics that provide cardiovascular and renal benefits in order to improve the prognosis, prevention and management of RDE in the future.
