Author(s): <p>Mustafa Tawfeeq Halboos, Marrwan Hisham Mohammed*, Ziyad Kamel Al Jenabi and Noor Hamad</p>
Refractive errors are frequently found among school children due to various factors such as genetics and lack of parental attention toward regular eye check-ups by an ophthalmologist. It is crucial to conduct visual examinations in schools to identify and address any eye-related issues promptly. Aim: The objective is to evaluate the level of refractive error and strabismus among students in two primary schools located in Babylon City, Iraq. Method: From October 20, 2021, to February 1, 2022, cross-sectional, retrospective research was conducted at two primary schools, Al-Nidal and Al, in Babylon, Iraq, for children aged 7 to 12 years. Result: One thousand twenty pupils. We excluded eight students from this study. They participated (2028 eyes) at two primary schools in the Iraqi city of Babylon. There were 422 male students (41.3 %) and 592 female students (57.9%), mean age was 9.7 ± 1.6 (range, 5-12) years. Congenital, acquired, and normal eyes were found in 78 (7.6%), 62 (6.1%), and 874 (85.5%) students, respectively (P<.001). We found emmetropic most common in two primary schools; myopia was more than Hypermetropia, astigmatism, and amblyopia was 80.0%, 9.0%, 7.2%, 2.9%, and 4.1%students, respectively. Conclusion: A study conducted in Babylon; Iraq revealed a high occurrence of uncorrected refractive errors in elementary school students. This finding highlights a significant health issue for young individuals, which calls for immediate action to address and rectify. Regular visual acuity tests should be conducted annually to identify and correct any refractive errors.
Loss of sight and visual impairment in childhood or primary school is more important and disabling than adult blindness, given its prolonged existence and permanent effects on developing eyes, which may lead to the development of amblyopia [1,2]. In children around the globe, refractive error leads to cause of poor vision which is one of the major causes of treatable visual impairment, accounting for approximately 80% of vision problems in children in the United States [3]. It will likely be higher in less developed countries. There is evidence that uncorrected error of refractivity is the leading cause of avoidable blindness around the globe [4]. Many factors play an important role in the refractive error prevalence, including the environment and age in the distribution and prevalence of the pattern of refractive defects. It ranges from less than 1 % of children in Tanzania to over 36.7 % in Malaysia. In addition, cases range from about 3% in South Africa to 15.8% in Chile [5,6]. In many of the world, refractive errors were and until now cause blindness, also the disease with refractive error to lead blindness and cataract of the lens until now reasons in vision poor [7]. Refractive errors are one of the five goals of the Global Program to End Avoidable Blindness, the initiative known as Vision 2020 was instituted by the World Health Organization (WHO) and the International Agency for the Prevention of Blindness [8]. Due to the various armed conflicts and socioeconomic and healthcare challenges faced by Iraq, it is imperative to gain insight into the ocular health and child personnel practices during their most vulnerable developmental stage. Primary educational institutions cater to students below the age of 12 years. Refractive errors, encompassing myopia (nearsightedness), hyperopia (farsightedness), and astigmatism, blur the clarity of vision by impairing the eye’s ability to focus light accurately onto the retina. Such visual distortions can hinder a child’s capacity to perceive classroom materials, leading to difficulties in reading, writing, and absorbing information presented on chalkboards or screens. Strabismus, commonly referred to as “crossed eyes” or “lazy eye,” arises from the misalignment of the eyes, disrupting binocular vision and causing problems with depth perception [9,10]. The refractive errors are defined as spherical or cylindrical based on the type of lens required to rectify them [10-24]. Inclusion Criteria: All students from the first to sixth class were included in the study. This comprehensive approach ensures that the study encompasses a wide range of age groups within the primary school setting, providing a holistic view of the prevalence of refractive errors and strabismus. Exclusion criteria: Students who had eye infections or traumatic eye diseases and did not submit their questionnaires during the screening, as well as those who were absent from school during the examination, were not included in the study. Data was analyzed using SPSS version 24 software. Descriptive statistics, including deviation and ratios, were generated using statistical tables. Relationships between variables were examined using correlation analysis. A p-value less than 0.05 was considered statistically significant. The statement of the problem was we missed gathering information on refractive errors in primary schools in southern Iraq due to war and life challenges.
The research program years of Mustaqbal University supported this study, but it did not receive a grant money from Al Mustaqbal University from the Foundation of Basic Research.
In this retrospective study, 1020 students were selected, and 2040 eyes were analyzed. Eight students and 16 eyes were excluded. The study followed the Declaration of Helsinki and was approved by the Mustaqbal University of Medical Sciences Research Ethics Committee (Opt.7/2023). Data collection occurred from October 20, 2022, to February 1, 2023, at two Babylon, Iraq primary schools: Al-Nidal and Al-Ajyall. Inclusion criteria: The study included students from the first to sixth grade. Exclusion criteria: Students with eye infections and traumatic eye diseases failed to provide their questionnaires during the day of screening, and those who were absent from school on the day of the examination were excluded from the study. Participants were aged 7 to 12 years. All students from both schools were included, while teachers and students with strabismus-related trauma or surgery were excluded.
The eyes underwent comprehensive evaluation, encompassing visual acuity measurement with the Log MAR chart at 6 meters, fundus examination, and both subjective and cycloplegic refraction assessments. For cycloplegic refraction, two drops of 1% cyclopentolate were administered to both eyes a minimum of 45 minutes before examination. These drops dilated pupils and eased ciliary muscle strain, aiding refractive status assessment via autorefractor and retinoscope. Participants were grouped based on their refractive errors: hyperopia, myopia, and astigmatism.
Hyperopia was defined by a spherical equivalent of ≥+1.00 diopters in one or both eyes, while myopia was identified by a spherical equivalent of ≥-0.75 diopters in one or both eyes. Astigmatism was established as a cylinder error equivalent of ≥0.50 diopters. This categorization facilitated the precise classification of patients’ refractive conditions.
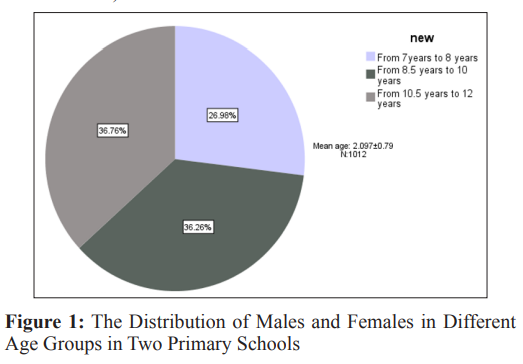
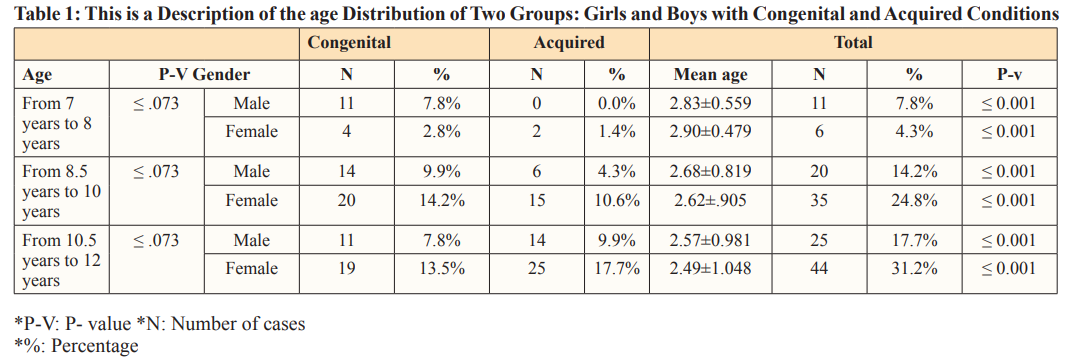
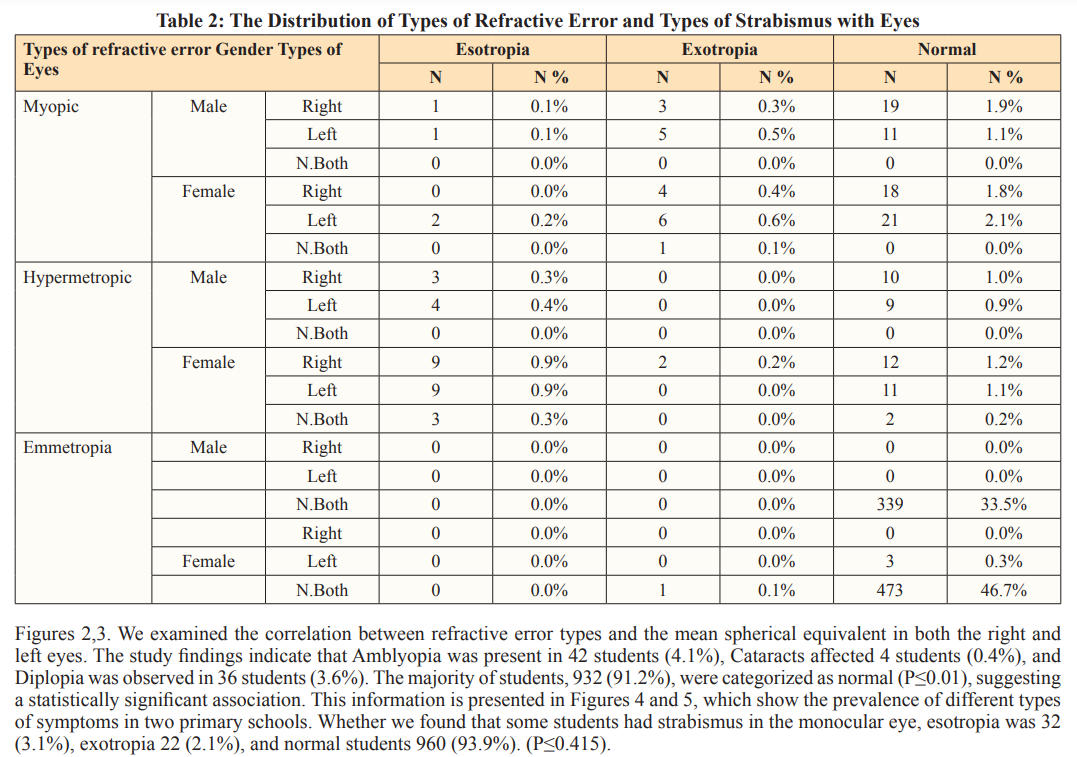
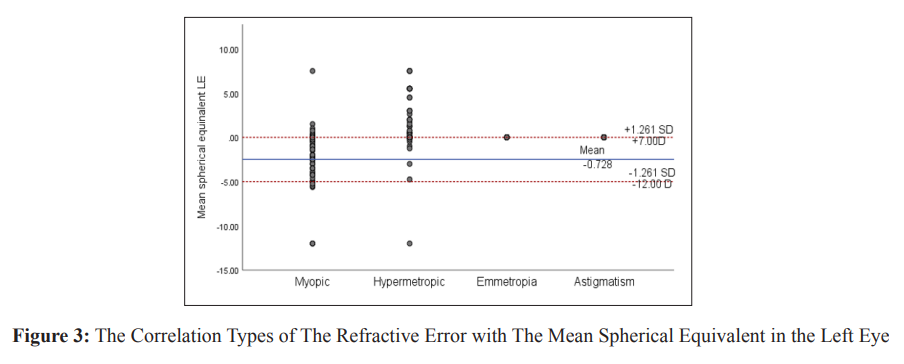
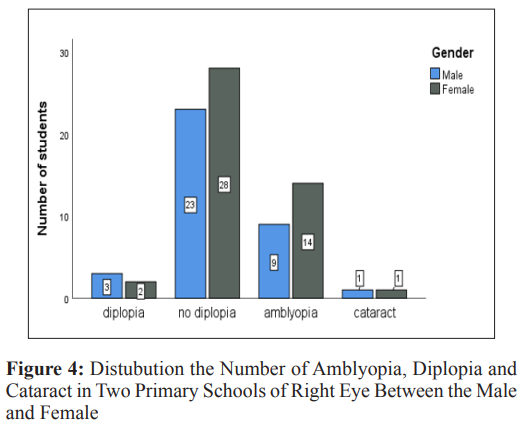
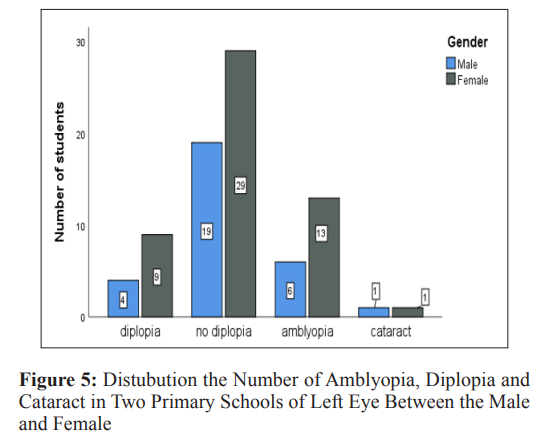
A total of 1,024 students participated in the study, with eight students excluded. The study included 2,024 eyes from two primary schools located in the city of Babylon, Iraq. Of the participants, 422 were male (41.7%) and 590 were female (58.3%), Figure 1, with a mean age of 9.7 ± 1.6 (range, 7-12) years. Congenital, acquired, and normal etiologies were found in 78 (7.6%), 62 (6.1%), and 874 (85.5%) students, respectively(P<.434). Table 1 describes the subjects’ ages in two groups of girls and boys with congenital and acquired p-values was ≤0.001. Table 2 shows the distribution of types of refractive error among studies in primary school. In this study, the myopic, hypermetropic, astigmatism, and emmetropia in boys were 40 (3.9%), 26 (2.6%),17 (1.7%), and 339 (33.4%), respectively. Also, the myopic, hypermetropic, astigmatism, and emmetropia in girls were 52 (5.1%), 48 (4.7%), 13 (1.3%), and 479 (47.2%), respectively. (P≤ 0.561) (under consideration)
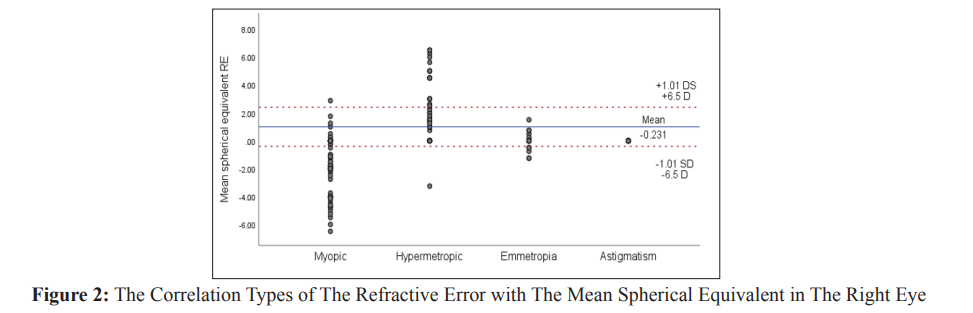
This cross-sectional (retrospective) study was conducted to assess the occurrence of refractive errors among primary school children in Babylon, Iraq. The findings revealed a prevalence of 19.3% for refractive errors. Among these, myopia emerged as the most prevalent condition, accounting for 47.0% of all identified refractive errors.
Our study encompassed a sample size of 1014 students, which is notably larger compared to Mohammed’s study involving 680 students and Rafea A’s study with 592 students [11,12]. Moreover, our study revealed a distribution of 41.7% male and 58.3% female participants. However, in Rafea AF’s study the male-female distribution was 51.9% and 48.1% respectively, and in Noor H A’s study it was 44.8% male and 55.2% female [13,14]. These discrepancies in percentage distributions in our study could be attributed to the selection of a more extensive sample size. Indeed, the actual prevalence of myopia among schoolchildren in our study was determined to be 19.3%. It’s worth noting that our findings differed from those reported in the study conducted by MUKAZHANOVA, where a higher prevalence of refractive error, specifically 31.6%, was observed [15]. In this study conducted in Babylon, Iraq, the occurrence of refractive error was determined to be 18% among students from two primary schools. This prevalence rate is lower than the 26.73% reported in a study involving college students in Iraq [15-20]. However, the prevalence rates found in other studies, such as the one in Kathmandu, Nepal (8.1%), Chile (8.8%), and by Zhao J (11.3%), were more in line with the findings of our study [14,5,16]. Furthermore, the prevalence of myopia, at 9.1%, closely resembled that reported among the Malay population in East Malaysia (6.0%), as well as the study by Murthy GV (8.4%) [17,18]. However, the myopia prevalence in our study was higher than the study conducted in Kathmandu, Nepal (4.3%). Similarly, the prevalence of hypermetropia, at 7.2%, is closely aligned with findings from the study by Murthy GV (6.2%) and Chile (7.2%). Discrepancies were noted in other studies, such as Nepal (1.4%) and Wadaani FA (1.7%) [14,18,19].
The prevalence of astigmatism, at 3.0%, closely resembled the findings from the study in Nepal (2.4%), while diverging significantly from the study by Rose KA (15%) [14, 20]. These may include the definition of study populations, definition of myopia, hyperopia, and astigmatism, methods of measurement, and the types of environments- all factors considered. However, as only students with visual acuity of ≤ 0.30 (6/12) were collected, many students with a low degree of refractive error may have gone undetected. Hyperopic children may compensate by accommodation, while some myopic children may squint, masking the actual level of poor visual acuity [21,22].
The factors associated with refractive errors in primary school children in Babylon were age, hours of reading per day, computer use, and siblings’ history of wearing glasses. Gender and parental history of eyeglass-wearing were not significantly associated with refractive errors.
Our study was cross-sectional, so we could not establish a causal relationship between the associations we observed in the risk factor analyses. Moreover, our measurements were taken once at the beginning of the school year, in the fall. It may have a biased effect in reducing the prevalence of myopia because children may spend more time outdoors in the warm season, especially during the summer holidays, with greater exposure to natural daylight [23, 24].
This cross-sectional (retrospective) study selected 2048 eyes from 1024 students; in this study, we do not a significant difference in refractive errors between boys and girls due to (P=0.561). We found the prevalence of myopia more than hypermetropia in primary schools, so esotropia was a little more than exotropia, but their percentage is small in primary schools. Also, this study examines the effect of age and gender on the type of refractive error, and no associations were found. These findings highlight the importance of an appropriate testing program for school-age children.
We want to thank the Babylon Education Directorate and the school staff for their assistance in organizing the study. We thank the reviewers and editor for their careful review and insightful comments. I thank the Dean of Mustaqbal University for agreeing to do this research and supporting us.
1.Flaxman SR, Bourne RR, Resnikoff S, Ackland P, Braithwaite T, et al. (2017) Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. The Lancet Global Health 5: e1221-e1234.
2.Michaeline I, Sheriff A, Bimbo A (2016) Paediatric refractive errors in an eye clinic in Osogbo, Nigeria. Ethiopian journal of health sciences 26: 147-154.
3.Lou L, Yao C, Jin Y, Perez V, Ye J (2016) Global patterns in health burden of uncorrected refractive error. Investigative ophthalmology & visual science 57: 6271-6277.
4.Pi L H, Chen L, Liu Q, Ke N, Fang J, et al. (2012) Prevalence of eye diseases and causes of visual impairment in school- aged children in Western China. Journal of epidemiology 22: 37-44.
5.Chia E M, Wang JJ, Rochtchina E, Smith W, Cumming RR, et al. (2004) Impact of bilateral visual impairment on health-related quality of life: the Blue Mountains Eye Study. Investigative ophthalmology & visual science 45: 71-76.
6.Recko M, Stahl ED (2015) Childhood myopia: epidemiology, risk factors, and prevention. Missouri medicine 112: 1-116.
7.Harrington SC, Stack J, O’Dwyer V (2019) Risk factors associated with myopia in schoolchildren in Ireland. British Journal of Ophthalmology 103: 1803-1809.
8.Wen G, Tarczy Hornoch K, McKean Cowdin R, Cotter SA, Borchert M, et al. (2013) Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthalmology 120: 2109-2116.
9.Delcourt C, Korobelnik J F, Buitendijk GH, Foster PJ, Hammond CJ, et al. (2016) Ophthalmic epidemiology in Europe: the “European Eye Epidemiology”(E3) consortium. European journal of epidemiology 31: 197-210.
10.Holden BA, Sulaiman S, Knox K (2000) The challenge of providing spectacles in the developing world. Community Eye Health 13: 9.
11.Mohamed J, Mohamed J (2018) A thesis of clinical- epidemiological study of visual acuity among students of three colleges in ALMustansiriya University 1-10.
12.Rafea F E (2019) Association between Strabismus and Refractive Errors among Preschool Children in Fallujah, Iraq 10: 1-509.
13.Oecd (2014) Does Homework Perpetuate Inequities in Education? OECD Publishing 1-4.
14.Nepal BP, Koirala S, Adhikary S (2012) Ocular morbidity in school children in Kathmandu. Br J Ophthalmol 87: 531-534.
15.Mukazhanova, Ainagul (2022) Prevalence of refractive errors and risk factors for myopia among schoolchildren of Almaty, Kazakhstan: A cross-sectional study. PloS one 6: e0269474.
16.Zhao J, Pan X, Sui R, Munoz SR, Sperduto RD, et al. (2010) Refractive error study in children: results from Shunyi district, China. Am J Ophthalmol 129: 427-435.
17.GHOSH, Deva (2010) Geophysical issues, and challenges in Malay and adjacent basins from an E & P perspective. The Leading Edge 4: 436-449.f
18.Murthy GV, Gupta SK, Ellwein LB, Munoz SR, Pokharel GP, et al. (2012) Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci 43: 623-631.
19.Al Wadaani FA, Amin TT, Ali A, Khan AR (2012) Prevalence and pattern of refractive errors among primary school children in Al Hassa, Saudi Arabia. Glob J Health Sci 5: 125-134.
20.Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, et al. (2018) Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 115: 1279-1285.
21.Mohammed, Iman Ahmed, AL Diwan, Jawad K, Mohammed Anwar Ahmed (2022) Prevalence of refractive error among a sample of children from two primary schools from Al-Rusafa in Baghdad 125-134.
22.Fayyadh, Rafea Allawi, Abady Noor Hussain (2020) Prevalence of Uncorrected Refractive Errors Among the Internally Displaced Schoolchildren in Iraq. Medico-legal Update 1: 1-45.
23.Rusnak S, Salcman V, Hecova L, Kasl Z (2018) Myopia progression risk: seasonal and lifestyle variations in axial length growth in Czech children. Journal of Ophthalmology 6: 5076454.
24.Mohammed M H, Halboos M T, Al Jenabi Z K, Khorrami Nejad M (2022) The clinical findings of different refractive errors for students studying at college of medical technology, Al-Mustaqbal University in Babylon City of Iraq from 18 to 20 years. International Journal of Health Sciences 6: 2545-2551.
View PDF