Author(s): <p>Jacob Sheehama</p>
This study sought to describe the level of severity of depressive symptoms in adults with diagnosed diabetes. Primary objective was calculating the prevalence of depressive symptoms with secondary objectives of severity and contributing factors to development of depressive symptoms. A cross-sectional study design was used, focussing on the relationships between the outcome of disease (depression) and exposure (factors contributing to development of depression). A three-part questionnaire on demographics, health parameters and depression symptoms was given to adults with diagnosed Diabetes at the Katutura State Hospital Outpatient Department over the course of six weeks, chosen by systemic sampling. Patients on first visit (undiagnosed DM) or with Gestational Diabetes were excluded from the study. Of the 113 individuals who met the inclusion criteria, 101 were included in this study. Only 2 patients (1.98%) had no symptoms of depression whatsoever, the rest categorized into having mild, moderate and severe symptoms. Severe depressive symptoms were present in 19.8% of the total group (20/101), with a male to female ratio of 2:3 (Risk Ratio - 0.98, p-value 0.48), with 40% above the age of 65 (RR - 1.57, p-value 0.14), and 80% had Type 2 Diabetes Mellitus (RR - 1.85, p-value 0.11). Socio-economic factors such as no formal schooling and only having pension as a sole source of income, were most common in the group with severe depression. Health care workers should be able to identify signs of depression and refer accordingly, as psychosocial support is needed in patients with chronic, often incurable conditions.
Diabetes is a group of metabolic disorders that are characterized by chronic hyperglycaemia1. It is classed as a non-communicable lifestyle disease, as it is not caused by any infection, but by different contributing factors. These factors are genetic, nutritive and environmental. Diabetes is usually a primary, which is divided into Type I (formally known as insulin-dependent Diabetes Mellitus) caused by an autoimmune disorder of the pancreatic beta cells (respinsible for insulin production) and Type II (non-insulin dependent Diabetes Mellitus) which is due to insulin resistance (body is desensitized to the effect of insulin). Non-Communicable Diseases (i.e. Cardiovascular diseases, Cancers, Chronic Respiratory Diseases, Diabetes and Other NonCommunicable Diseases) are on the rise in Namibia, accounting for 41% of total deaths in all ages and both sexes4. Due to the heavy focus on Infectious Diseases (TB, Malaria, HIV/AIDS) while essential (accounting for 47% of deaths), has led to reduced visibility for Non-Communicable Diseases and its management. It is for this reason that the current study was conducted. Patients with lifelong conditions such as diabetes that have no cure and must be constantly controlled may have detrimental mental health conditions due to the chronicity. Such chronic diseases have a major impact on the quality of life, specifically the psychosocial aspects. By identifying mental health symptoms in patients with Non-communicable diseases, one will be able to pinpoint the main cause (whether due to the general medical condition or a primary mental condition) and treat accordingly, improving the quality of life immensely. Mental health is a neglected area in the Namibian Health System, with there being a paucity of epidemiological data on mental illnesses in Namibia5. The primary outcome of this study is the prevalence of depression in patients with diabetes, with its severity and the causative factors thereof being the secondary outcome.
A cross-sectional study design was used, focussing on the relationships between the outcome of disease (depression) and exposure (factors contributing to development of depression). The inclusion criteria of the defined population was adults (persons over the age of 18) with diagnosed diabetes (specifically Type 1 and Type 2 Diabetes) coming for follow-up at Katutura State Hospital. The group was approached during their regular follow-ups and the consent form was given to them prior to officially enrolling them into the study. Patients with Gestational Diabetes or came for first visit (not yet diagnosed Diabetes) were excluded from the study.
The questionnaire was based on different scales used to diagnose depression according to the DSM (Diagnostic StatisticManual) V12classification of depression/mood disorders, namely the Hamilton Depression Rating Scale10, Patient Health Questionnaire11, Major Depression Inventory & Hospital Anxiety and Depression Scale. A scoring system from the questionnaire was used to categorise the patients into no, mild, moderate and severe depressive symptoms. Various factors were also included to see which of these led to the development of depression (gender, age, level of education, and employment status)
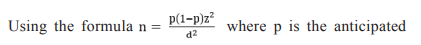
population proportion, d is the precision required on either side
of the proportion, and z refers to the cut-off value (is 1.96 at 95%
confidence interval,) n is the estimated sample size. By using
the formula above, with p = 0.5 (50% from the hypothesis), z =
1.96 and d = 10% = 0.1 (for a range of 45% to 55%), the sample
size is therefore 96.04 = 96. To account for possible refusal/
withdrawal rate of 10%, the proposed sample size will be 105.6
= 106. Individuals were chosen by systemic sampling.
Data was collected from all participants that fit the inclusion
criteria (Age 18 years and above with previous diagnosis of
Diabetes Mellitus coming for follow-up), at the Katutura State
Hospital Outpatient Department over the course of six weeks (from
first week of April to second week of May 2018), on Tuesdays
and Thursdays. A total of 113 individuals fit the inclusion criteria,
but only 101 answered the questionnaire to completion, with
seven questionnaires returned incomplete and five individuals
who refused to take part in the study. Main reasons for refusal
was due to language barriers (questionnaire was in English, with
only Afrikaans and Oshiwambo translators available) and the
content of some questions. Many were uncomfortable commenting
on suicidal ideations, causing them to withdraw from the study.
The data from these patients were omitted from the final results.
Of the 101 participants, majority were female (60%, 61/101) [Figure 1], mean age of 54.05, the most common age group were individuals above the age of 65 (30% - 30/101), with Type 2 Diabetes being the most common diagnosis (70% - 69/101) [Figure 2]. Average BMI was 29.1, Hypertension the most common comorbid disease, and sight problems the most common complication, however 70% of participants did not present with complications.
Of the 101 individuals interviewed, only 2 patients (1.98%) had no symptoms of depression whatsoever (score 0/30), with the remaining 99 having either mild (score 1 - 10), moderate (score 11 - 20) or severe (score 21 - 30) depressive symptoms [Figure 3]. There were 38 (37.6%) who had mild depressive symptoms, of whom 18 (47%) were male, 20 (53%) were female with the most common age group 46 - 55 years (32%). Moderate depressive symptoms was present in 41 participants (40.6%), 13 (32%) male and 28 (68%) female, most common age group 65+ (41%). Severe depressive symptoms were only present in 19.8% of the total group (20/101), with a male to female ratio of 2:3 (Risk Ratio - 0.98, p-value 0.48), with 40% above the age of 65 (RR - 1.57, p-value 0.14), and 80% had Type 2 Diabetes Mellitus (RR - 1.85, p-value 0.11). [Figure 4,5,6] Of note, both moderate and severe depressive symptoms were represented in every age group. [Table 1, 2].
In terms of socio-economic demographics, those with severe depressive symptoms were mostly pensioners (50%), with no formal education (45%), despite majority of the group (38/101 - 37.6%) reported to have attended up to secondary school. Severe depression was also found to be more common in individuals who used insulin alone (45%) compared to those who used oral medication alone (35%).
Based on the results of the study, many of the participants had (98%) at least one depressive symptom, however depression is only clinically significant if five or more symptoms to be diagnoses as a depressive episode according to DSM V12. This does however show that diabetes does have some psychological effect. Majority of the participants were over 65 years of age and pensioners, who had some form of morbidity (vision impairment, coexisting hypertension).
Socio-economic factors such as no formal schooling and only having pension as a sole source of income, were most common in the group with severe depression. This could tie-in with populations that are at highest risk for diabetes, such as racial and ethnic minorities and persons from low socioeconomic backgrounds, experiencing environmental exposures (e.g., poverty, stress) that increase risk for mental illness, interfere with self-care and compromise medical management [13].
The DAWN (Diabetes Attitudes, Wishes and Needs) Study was the world’s largest international psychosocial study in persons with diabetes, conducted by Novo Nordisk in partnership with the International Diabetes Federation in 2001. It included 5000 people with diabetes and 3000 diabetes healthcare professionals across 13 countries. The results of the DAWN Study showed that as many as 41% of the patients had poor psychological well-being, with only 10% of whom received psychological care6. Cross-sectional studies of elevated depressive symptoms suggest that depressive symptoms appear to persist for prolonged periods (e.g., 12-18 months), but no longitudinal studies have documented duration of diagnosed depression episodes in T1D or T2D samples to date [8, 13].
Of note severe depression was more common in patients who used insulin alone as opposed to oral antidiabetic medication, possibly indicating increased psychological stress due to the route of administration as well as its maintenance (insulin requires refrigeration).
Some weaknesses noted during this study was the bias in sex distribution. Efforts should have been made to even out the distribution, as it skews the results to having a female predominance, which may not be a true reflection of the prevalence of depression. P - values were all more that 0.05, indicating that there was no statistical significance in terms of relative risk of advanced age, sex and diabetes type in the development of depression. It was also difficult to analyse data regarding the question of “Distance/ Time from nearest health facility” in the data collection tool as many of the participants had difficulty answering the question in the units given.
The need for good psychosocial support for patients with chronic, often incurable diseases is very important. As per the WHO definition of health, a “state of complete physical, mental, and social well-being, and not merely the absence of disease or infirmity”, mental health care should be included in follow-up visits for patients with diabetes. It is also important for health care workers to be able to identify signs of depression and refer accordingly, and be careful not to dismiss the patient or the family’s concerns [14]. Patients should be encouraged to practice self-care, as it will help the patient have a form of control over the diseaseand prevent further morbidity. A holistic approach including social workers, dieticians, psychologists and psychiatrists along with the primary care givers could also prove to better the patient’s quality of life.
Mental illness has some negative connotations culturally in the African context, leading many to not address it in themselves or in family members, shown by refusal of some participants to answer questions on suicidal ideations and attempts. With the added stress of disease, there is a higher risk of development of mental illness especially in patients with chronic diseases that affect their quality of life. In conclusion, emphasis should be placed on inquiring about psychological stresses in patients with chronic conditions, and may also be important for palliation if condition is incurable. This task falls not only on the physician encountering the patient, but also the caretakers, and the health system at large. While this study had its limitations, it provides a door for broader research in the topic [[1-7] & [9-12]].
