Author(s): <p>Jihane Hamdaoui*, Samir El Mazouz, Noureddine Gharib, Abdellah Abbassi and Jawad Hafidi</p>
Cutis verticis gyrata (CVG), or vorticella pachyderma of the scalp, is a rare and progressive condition of the skin of the scalp and/or face. It is characterized by hypertrophy and hyperlaxity of the skin forming similar folds on the surface of the cerebral cortex [1]. These folds can cause aesthetic, social and functional discomfort (maceration, infection) [2-4].
We present the case of an 18-year-old female patient suffering from primary essential CVG since the beginning of adolescence (12-13 years) on the scalp and was progressively worsening. Only the scalp was affected in the form of hypertrophy and hyperlaxity of the skin responsible for longitudinal and transverse excess. The patient’s request was motivated by aesthetic and social discomfort, causing a complex pushing her to permanently wear a scarf.
Upon questioning, she presented no family history or chronic pathology that could be the cause of a secondary form of CVG. No triggering factor was identified. There was no ongoing treatment and the patient’s intellectual abilities were normal.
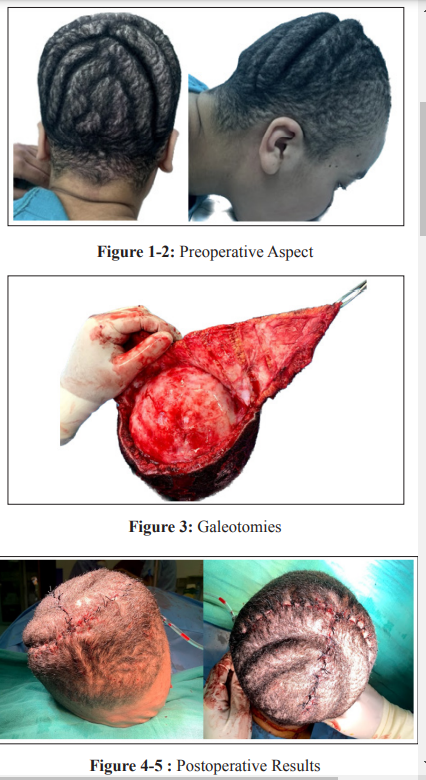
On clinical examination, the folds appeared to be formed from alternating areas of normal and very thick skin and preferentially affected the occipital region and the vertex and were responsible for a retreat of the hairy implantation region. (Figure 1-2).
AT-shaped surgical excision on the vertex and the occipital region was performed. The patient was placed in the prone position on a neurosurgical headrest. The procedure was carried out under general anesthesia. After infiltration of Merkel’s space with adrenaline serum, the skin and galea were easily peeled off according to the established route. Galeotomies were performed (Figure 3) next to the folds in order to obtain maximum skin expansion in the anteroposterior plane followed by resections in order to reduce the excess in a longitudinal and transverse plane. Careful hemostasis was achieved. Closure was carried out in two planes (deep and superficial dermal), on a suction drain (Figure 4-5). The postoperative course was simple, with the drain removed after 24 hours. The patient was very satisfied with the result.
This pathology was first reported by Alibert in 1837 under the term “cutis sulcata” [5]. In 1907, Unna gave it the name CVG, commonly accepted since [6]
Three forms of CVG can be distinguished CVG secondary to chronic metabolic, inflammatory, respiratory, cardiac, endocrine, hepatobiliary and paraneoplastic forms, or even iatrogenic pathologies [7-15]. following treatment with Minoxidil [16]. CVG is also present in pachydermoperiostosis (or chronic hypertrophic osteoarthritis). Chronic traction of the scalp has even been described as the cause of CVG [17]. This form is the most common and more frequently affects the face in association with involvement of the scalp. It preferentially affects men with a sex ratio of 5:1; the primitive CVG, much rarer, whose origin is genetic with indeterminate transmission [7,11,18]. It can be essential or non-essential: the non-essential form is associated with neurological and/or ophthalmic abnormalities (mental retardation, epilepsy, congenital cataract, microcephaly, encephalopathies, other neurological malformations) the essential primitive form preferentially affects males and begins at the end of adolescence [2-4,7,15,18]. Only 16 cases of primary essential CVG treated surgically are reported in the literature.
Our patient also presented with a form of essential primary CVG.
These three forms have in common an attack on the scalp in the form of hypertrophy and hyperlaxity of the skin causing folds in both axes, transverse and longitudinal. They progress slowly and have a recurrent nature after surgery. Medical treatment with isotretinoin has been proposed but proved to be of low effectiveness [19]. Surgery is the morphological treatment of choice for this condition, but does not prevent the progression of the disease. Some authors have recommended therapeutic abstention for as long as possible. Surgery seems, for our analysis, indicated when the patient requests it, whether motivated by aesthetic, psychological or functional discomfort (maceration, infection). The excision plan must take into account four main elements: the position of the scars must take into account the progressive nature of the disease to authorize future excisions; the excision scheme must absorb an excess in both axes; the plan must be able to absorb excess skin over the entire scalp (frontal, parietotemporal and occipital) during the first and future interventions; the incisions must create flaps with reliable vascularization. Kara reports the case of a patient treated following two bicoronal incisions [20]. Al-Malaq et al, as well as Horch et al, describe similar results by direct excision of skin folds [21]. Radwanski et al, report a “fleur de Lys” excision pattern, thus taking into account the two components of excess skin [22]. Snyder describes a case treated with skin expansion, wide excision and rotation flaps [23]. Finally, Misirlioglu et al, report the treatment of a case by circular excision and helical flaps [24].
We adopted the T pattern, which made it possible to improve the appearance of the patient’s scalp as well as her forehead. The longitudinal incisions of the galea (galeotomies) made it possible to obtain a slight expansion of the skin and therefore an additional skin resection, without compromising the vascularization of the flaps.
Primary CVG, or vorticella pachyderma of the scalp, is a rare and progressive disease causing social and aesthetic disability. This disease requires a clinical and paraclinical assessment to eliminate non-essential secondary and primary forms. The treatment is surgical, by excision of the most wrinkled skin areas and retensioning of the scalp in a longitudinal and transverse plane. Excisions must take into account the vascular anatomy of the scalp and the iterative nature of the surgery. They can be helped by additional incisions in the galea next to the residual folds. Surgical treatment seems indicated to us when the patient requests it.
