Author(s): Nirali Shah*, Vidhi Shah, Falguni Goswami and Roopam Gidwani
Introduction: Bone marrow examination is an important diagnostic tool to evaluate various hematological and non-hematological disorders. The two most important techniques used for the diagnosis are bone marrow aspiration and bone marrow biopsy which play complementary role with each other when performed simultaneously.
Aims and Objectives: Study was done to compare the results of BMA and BMB and by that to prove the complementary role of both techniques to each other.
Material and Methods: We evaluated total 74 cases in central laboratory, department of pathology, at tertiary care centre. All aspirations were stained by giemsa and iron stain while all biopsy were stained by routine H&E stain. Reticulin stain and IHC markers were used as and when required.
Result: Out of total 74 cases, 40 cases showed positive corelation between these two techniques (54%). In two cases aspiration was not possible. In 8 cases biopsy was not done. 4 cases showed crushing artefact in BMB while 3 cases of aspiration were either diluted or dry tap. In all these cases diagnosis became possible by the alternate technique. BMB replaced BMA and vice versa as and when required.
Conclusion: BMA and BMB are complementary procedure which yields extra support in diagnosing various hematological and non hematological disorders when one or other technique fails due to some reason.
Bone marrow examination is a formidable weapon in the clinician’s diagnostic armamentarium to hit an unsuspected diagnosis when other test results turn out to be non-contributory or inconclusive during the evaluation process [1, 2]. It is a useful investigative tool for the diagnosis of many hematological and nonhematological disorders [3].
Bone marrow examination may be performed by two methods: Aspiration and trephine biopsy. Bone marrow aspiration (BMA) is simple, reliable, and rapid method of marrow evaluation. It provides information about the numerical and cytological features of marrow cells. These cells are also well suited to further examination by cytogenetics, molecular and flow cytometric methods. However, BMA has low sensitivity in detecting solid tumour metastasis and lymphoma involvement [4, 5].
Bone marrow trephine biopsies (BMB) provide excellent appreciation of spatial relationships between cells and of overall bone marrow structure. It is required in conditions such as inadequate or failed aspirate, assessment of cellularity and bone marrow architecture, suspected focal lesion (for example, suspected granulomatous disease, or lymphoma) and bone marrow fibrosis [2].
Nowadays, aspirate and trephine biopsy specimens are considered complementary and when both are obtained, they provide a comprehensive study of bone marrow.
With advent of new technologies such as flow cytometry, immunohistochemistry (IHC) and molecular techniques combined analyses is useful in achieving more accurate and informative diagnostic data in some diagnostically challenging cases. We conducted this study with the objective of comparing the accuracy as well as complementary role of BMA with BMB in the diagnosis of various hematological and non-hematological disorders.
We retrospectively reviewed a total number of 74 cases of bone marrow examination received in the department of pathology of our institution from Jan 2019 to August 2020. Patients were reviewed irrespective of age and sex. The clinical history and findings of physical examination were noted. All the necessary investigations including complete blood count, peripheral smear examination, thick smear for malarial parasite, sickling test, reticulocyte count, coagulation profile, serum investigations and radiological investigations were carried out before doing BM examination. Indications and complications of BM examination were explained to the patient but also assured for safety, simplicity and usefulness of the procedure. Written consent was taken from relative or patient himself
One ampoule (0.5 mg) of atropine was given 15 minutes before procedure. BM aspiration was done from posterior superior iliac spine followed by biopsy using Jamshidi-Swaim needle. The technique employed was the same as that described by Mc Farland et al. From aspirated marrow particles one crush smear and one thin spread preparation were prepared at bedside. Biopsy core was put in neutral formal saline .In the laboratory particle crush smears and thin spread smears were prepared from the aspirate collected in citrate bulb and fixed for 20 minutes with methanol and stained with the combination of Leishman and Giemsa stain for 12 minutes. After 24 hours biopsy core was transferred from neutral formal saline to EDTA solution and kept for 48 hours for decalcification. All the biopsies were routinely processed. The sections were stained with Harris’s Haematoxylin and Eosin for light microscopic examination. Prussian blue staining of aspirated smears of all cases was done. Aspirate smears and biopsy sections were examined microscopically. The histopathology findings and the diagnosis made on the biopsies were compared with the findings on the bone marrow aspirate and diagnosis [6].
Total 74 cases of different hematological and non-hematological indications were examined. Out of these, in two cases aspiration was not obtained while in 6 cases there was failure in obtaining BMB. So finally we had total 72 cases of bone marrow aspiration and 68 cases of bone marrow biopsy which were evaluated to reach the diagnosis. Out of these 74 cases, megaloblastic anaemia was the commonest cause of pancytopenia (11 cases) followed by aplastic /Hypoplastic anaemia (10 cases) in aspiration study. The highest corelation was seen with Hypoplastic/aplastic Anaemia (90%) (Fig 1) followed by megaloblastic cases (82%) (Fig 2) in BMB. There were 2 diluted marrow on aspiration out of which one turned out to be Immune Thrombocytopenia (ITP) and other was normal on biopsy examination. One case was dry tap on aspiration which was diagnosed as Chronic Myeloproliferative Disorder (CMPD) - either CML or Polycythaemia Vera on bone marrow biopsy diagnosis. One case confirmed as B cell Lymphoma (NHL) on biopsy which was diagnosed as Chronic lymphoproliferative disorder on aspiration and this diagnosis was confirmed by Immunohistochemistry. There was a case of MDS which was confirmed by both aspiration and biopsy

Figure 1
Figure 2
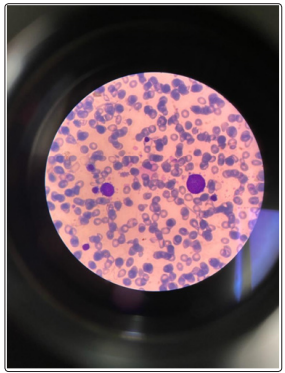
Figure 3
Bone Marrow examination play a key role in case of various hematological as well as non hematological diagnosis. We attempted this study to decide the complementary role of BMA and BMB and its utility in various disorders. Question concerning the efficacy of bone marrow aspiration over bone marrow biopsy has now got abolished when we compare these two techniques by their results. Bone marrow aspiration and biopsy using standard staining procedures, fixation, embedding and cutting techniques, generally complement each other with the aspirated smear being primarily used for cytologic details while biopsy sections mainly useful for cellularity, fibrosis, architectural pattern, metastatic deposits and from the same tissue we can go for Immunohistochemistry. These procedures are also useful for follow up of the patients undergoing chemotherapy [7]. Dry tap or blood tap is usually because of some pathology in the marrow and rarely because of faulty techniques. Bone marrow trephine is mandatory in such cases. Nowadays both specimens are routinely obtained at the same time and usually same site [8]. In this study we performed both the procedures simultaneously. There was 66% positive corelation between BMA and BMB which was 61.25% in a study done at medical college, Pondicherry [9]. In a study done by Manjit Kaur et al, positive corelation between BMA and BMB was 23/50 I .e 46% [10]. In our study, out of 74 total cases, in 6 cases biopsy was not possible either due to patient did not give consent for biopsy or due to porosity of bone. In 8 cases biopsy report was inconclusive while in 4 cases biopsy revealed no pathology. In all these cases diagnosis was possible only by BMA. Two cases which was diluted on aspiration and one with dry tap on aspiration came out with some diagnosis on BMB. The commonest hematological disorder in present study was Hypoplastic anaemia which was corelated by 90% between BMA and BMB. This was similar with the study done at Nobel Medical ,College while the study done by Parajuli et al Megaloblastic Anaemia was the most common diagnosis and study done by Vidisha Mahajan et al, Nutritional Anaemia was the most common diagnosis [11-13]. In this study there was one case of MDS which was diagnosed both by BMA and BMB (100%) which was similar in a study done by Pampa Ch Toi [9]. Leukemia (acute and chronic included) showed 71%corelation (5/7 cases) which was little more than in the study by Pampa Ch Toi [9]. in which there was 62.5% correlation (5/8 cases). We encountered a case of CMPD diagnosed on BMA which concluded by BMB as NHL and confirmed by IHC. In a study by Noble Medical College, a single case of NHL was diagnosed both on BMA and BMB, where as in study done by Vidisha et al much of the cases could not be diagnosed on the BMA alone, which stressed out point that both aspiration and biopsy should be done in case of suspected NHL [11, 13]. In one study by Pumpa Ch Toi, all 3 cases of Hodgkin’s lymphoma were diagnosed by BMB alone [9]. One patient was clinically suspected to have tuberculosis, but BMB showed Hodgkin’s disease. BMA showed reactive marrow. In a study done by Donald et al, 63% of metastatic carcinoma was only found to be positive in BMA [14]. A single case of Metastasis diagnosed on aspiration showed infarcted marrow in this study which could be comparable in a study done by Pumpa Ch.Toi [9]. In this study, there was a case of Granulomatous inflammation diagnosed by BMA in a patient of HIV infection, which was concluded the same by BMB. In a study by Pampa, 8/10 cases of granulomatous inflammation were diagnosed by BMB alone [9]. In this study, there was a case of sickle cell anaemia. BMA showed Parvovirus B19 infection, but BMB showed erythroid hyperplasia only. So only by BMA we could make a diagnosis in this case. As we mentioned in our study, the problem could be either in BMA which was dry or diluted or BMB which could be inadequate to report or showed crushing artifact. Ultimately with combining these two techniques, we could reach the diagnosis.
BMA and BMB are the procedures performed simultaneously nowadays. They complement each other. As experienced by us as well as different studies mentioned here, BMA are mainly used for evaluation of different conditions presented with pancytopenia, as it reveals cell morphology as well as iron staining. We came across causes of pancytopenia in form of megaloblastic anaemia /hypoplastic anaemia. To diagnose micro normoblastic anaemia, iron studies was helpful. At the same time BMB is mainly used to diagnose infiltrative lesions like leukemia, lymphoma or some metastatic non hematological disorder, because in such case we could able to apply IHC markers as well to confirm the diagnosis. Studies suggest that BMB is also useful for diagnosis of granulomatous lesions. While performing BMA and BMB simultaneously, employment of proper technique should be kept in mind so as to yield the maximum material and reduce discomfort to the patient by not repeating the procedure due to inadequate material as this a little painful invasive procedure.
