Author(s): Onah ES*, Anajekwu CC and Ezegwui IR
Background: Uncorrected refractive error (URE) is the leading cause of preventable blindness and global vision impairment (VI) with relatively high prevalence among school aged adolescents and children. Timely detection and correction may prevent the development of amblyopia, strabismus and enhance school success in these age group.
Aim: The aim of this study was to compare the refractive error measurements of Smartphone-based auto refraction with tabletop auto refraction and retinoscopy among adolescents attending eye clinic of Enugu State University of Science and Technology Teaching Hospital Parklane (ESUTTHP); Enugu, with a view to determining if portable Smartphone-based auto refraction can serve as a reliable alternative to tabletop auto refraction and Retinoscopy.
Methods: This was a hospital-based comparative cross-sectional study done over ten month period on 292 adolescents (584 eyes) aged 13-19 years with refractive errors attending eye clinic of the Hospital. Patients were selected by simple random sampling after which non-cycloplegic and cycloplegic refractive measurements of their eyes were performed using the three study instruments (Smartphone-based autorefractor (SBAR), Tabletop autorefractor (TTAR) and Retinoscope). The mean spherical values (SV) and spherical equivalent values (SEV) were determined and compared using ANOVA. Data entry and analysis were done using SPSS version 23.
Results: The mean age of the study participants was 16.6+0.76years, (age range 13-19years) comprising162 (55.5%) females and 130(44.5%) males; in the ratio of 1.3:1. Students constituted majority of the study participants 150 (51.4%). In non-cycloplegic state, 430 (73.6%) eyes were found to have refractive errors according to study definition (≥ 0.50 D); comprising 44 (7.5%) of myopia, 28 (4.8%) of hypermetropia, 264 (45.2%) of myopic astigmatism and 94 (16.1%) of hypermetropic astigmatism. But in cycloplegic state, 461(78.9%) eyes comprising 31(5.3%) of myopia,30 (5.1%) of hypermetropia, 320(54.8%) of myopic astigmatism and 80(13.7%) of hypermetropic astigmatism were found. The NETRA Smartphone-based auto refractor was found to measure refractive errors in adolescents as effectively as tabletop auto refractor both in non-cycloplegic and cycloplegic states but could not measure up to retinoscopy in both states.
Uncorrected refractive error (URE) remains an important cause of avoidable visual impairment and blindness globally despite being an easily correctible eye condition [1]. it can be readily treated with spectacles, making it imperative that effective strategies be developed for the assessment and control of this treatable cause of blindness [2]. Different methods of refractive error assessment have evolved over the years; with efforts geared most times towards comfort of patients, ease of operation by eye care professionals, affordability and accessibility of devices without compromising quality of care and accuracy of results [2].
Refractive error may be defined as a state in which the optical system of a non-accommodating eye fails to bring parallel rays of light to focus on the fovea [3]. It is caused by an incongruity between the axial length of the eye and the powers of the optical elements of the eye, so that compensatory lenses or other refractive treatment are required to produce a clear image [3]. Thus an individual’s refractive status results from an interplay in corneal power, lens power, anterior chamber depth, and axial length [4]. Refractive error can be strictly classified into three types: hypermetropia, myopia and astigmatism.
Hypermetropia (hyperopia) is the refractive state of the eye in which parallel rays of light from infinity are focused behind the retina [5]. Depending on the age of the person and the degree of hypermetropia, the manifestations can be asymptomatic or symptomatic. Small amount of hypermetropia especially in young individual is corrected by mild accommodative effort without any symptom [6].
However, symptomatic ones manifest with asthenopic symptoms which includes eye strain, tearing, photophobia, frontal or front temporal headache [5-6]. Myopia results when parallel rays of light are brought to focus in front of the retina and the secondary focal point of the eye forms a blurred image on the retina [6]. Poor vision for distance is the main symptom of myopia; however, asthenopic symptoms may occur in patients with small degree of myopia [5].
Astigmatism is that error of refraction where parallel light rays are not brought to a point focus but may be in front or behind the photosensitive layer of the retina with or without accommodation [6]. Symptoms include difficulty in focusing, transient blurred vision, dull eye ache, frontal headache and sometimes nausea as well as drowsiness which is especially marked in low astigmatism<1D [5]. Adolescence is a period in which one undergoes enormous physical and psychological changes [7]. The United Nations defines adolescent as a person aged 10–19 years: in effect, those who are in their second decade of life [8].
The visual health of adolescent individuals has been greatly affected in recent years by the social and technological changes that have been taking place globally. Giving the rapid urbanization occurring in most countries, characterized by a more technologically dependent educational system and growing popularity of electronic devices such as mobile phones, tablets and computers, children and adolescents are increasingly likely to take part in near activities. Therefore, with the increasing educational pressure, the prevalence of myopia has increased over the years from (1.78%) in 3-year-olds to (52.2%) in 10-year-olds [9-11]. Uncorrected refractive error with its attendant poor vision in this critical period of childhood and adolescence leads to difficulty in reading materials in soft or hard copies as well as those written on the black board. This adversely affects their learning, communication and general psychosocial behavior. Consequent on these, their education, occupation, health, socioeconomic status, and quality of life are affected with life-long consequences [12,13].
The technique of obtaining an accurate objective measurement of the refractive state of an eye using a retinoscope is known as retinoscopy. Retinoscopy remains a very vital tool in assessing and quantifying refractive errors even with the advent of auto refractors. But automated refractometer has become a popular method of refraction in recent years. This is due to the busy practices of eye care professionals, heavy patient load in clinics and screening camps, comfort of patients, relatively shorter testing time and learning curve [14].
To determine an accurate refractive result, all retinoscopic techniques which remains the gold standard for refraction essentially require that the accommodative status of the eye which is usually stronger in children and adolescents be at a minimum or temporarily disabled. This is achieved either by giving patient a far target, fogging with high power lenses or by using cycloplegic agents [15].
Though several attempts have been made to automate the process of refraction, over the last 200years with little success, a successful auto refractor became available in the last 30 years. This could objectively determine patient’s refractive status with an acceptable level of reliability. With the advent of technology, this equipment has become more sophisticated and increasingly precise [16]. The use of these auto refractors has increased due to their speed, reasonable accuracy, and repeatability. Digitalization and ICT development with its growing influence had continued to increase especially with the wide availability of mobile phones throughout human society. This has created opportunities for innovative solutions to be developed to meet the global demand especially in detecting and diagnosing of refractive cause of visual impairment [17].
The NETRA Smartphone-based auto refractive device was first developed by Eye NETRA Inc., Somerville at the Media Laboratory of Massachusetts Institute of Technology (MIT) USA in 2010 but became commercially available in 2015. It is a plastic, headset to which a user attaches a Smartphone, with an in-built software app, to the front of the plastic headset and then peeps through the headset at the phone’s display using one eye at a time. Patterns, such as separate red and green lines or circles, appear on the screen and the user turns a dial to align the patterns and then pushes a button to lock them in place. After eight interactions, the app calculates the difference between what the user sees as “aligned” and the actual alignment of the patterns. This reflects any refractive errors, such as myopia, hypermetropia, and astigmatism. The app then displays the refractive powers, axis of astigmatism, and interpupillary distance required for eyeglasses prescriptions [18]. It was developed to rapidly assess the refractive status of the eyes [19]. It became imperative to compare the emerging Smartphone-based auto refractor with conventional tabletop auto refractor as well as the traditional retinoscopy methods of refractive error assessment. This will provide adequate data that might support the use of Smartphone-based auto refractor in the refractive assessment of people living in developing, as well as in industrialized countries.
This was a hospital-based comparative cross-sectional study done over ten month period on 292 adolescents (584 eyes) aged 13-19 years with refractive errors attending eye clinic of Enugu State University of Science and Technology Teaching Hospital Parklane (ESUTTHP). Enugu state is one of the 36 states in Nigeria located in the south eastern region and the hospital provides tertiary levels of healthcare, including ophthalmic services. An average of thirty- two subjects per month (eight per week and two per working day) were recruited. A list of adolescents attending the eye clinic each day formed the study sample frame from which the study subjects were drawn. Inclusion was primarily from adolescents with one or more line of LogMAR chart improvement with pinhole visual acuity but those with media opacity, amblyopia, systemic diseases and other ocular pathologies other than refractive error were excluded. The study adhered to the tenets of the Helsinki declaration and the National code of health research on studies involving human subjects. Approval for the study was obtained from the ESUTTHP Health Research and Ethics committee before commencement of the study. Information obtained from the study was treated as private. Each subject was identified with a serial number which was known only to the researcher and the subject, thereby masking the identity of the subject. Upon obtaining informed consent, the visual acuity was checked using Log Mar chart. Socio-demographic data of subjects and a brief clinical history were taken, followed by a detailed ocular examination and diagnosis. Simple random sampling using balloting method was done on consenting subjects who were then enrolled into the study. Those enrolled in the study underwent non-cycloplegic retinoscopy, Smartphone-based autorefraction and tabletop auto refraction. After which cycloplegia was achieved using 1% cyclopentolate over 60 minutes (one hour), to dilate the pupil. Maximum cycloplegia was said to be established when pupil is dilated to ≥ 6mm or pupillary light reflex became absent [20]. Refractive measurements were then done with the three devices: retinoscopy, Smartphone-based auto refractor and tabletop auto refractor in that order. These tests were done by the principal researcher and two other research assistants and each person’s results were blinded from the other two to avoid bias. Three consecutive refraction measurements were obtained the same day for each eye of every subject without any gap in between for both the measurements of non-cyclplegic and cycloplegic test; then an average of the three measured values taken and recorded for each eye in the study proforma. If any two measurements of one instrument for each eye of the subject varied by more than 0.50 diopters (D), another set of three consecutive measurements were performed until the variation between each two measurements within one set became less than 0.50D [21]. This was to avoid inconsistency that may have resulted from poor cooperation of patient or operator’s technique during measurements; ensuring compliance with the research protocol and accuracy of the data collected [22].The principal researcher and each of the other research assistants were blinded on the results obtained from each of the devices and each of these researchers (2nd, 3rd and PI) separately; and independently submitted each test result (non cycloplegic and cycloplegic) to the respective data entrants who then entered the results of non-cycloplegic and cycloplegic into the respective Identifier forms to avoid bias at all stages of the tests.
The measured refractive values generated from the study were catego¬rized into two groups, non-cycloplegic and cycloplegic which was further categorized as spherical value (SV) for myopias and hypermetropias that are only spheres, spherical equivalent value (SEV) for myopic or hypermetropic compound astigmatism.
Data obtained were entered into Google data sheet, and then imported into the Statistical Package for Social Science (SPSS) version 23.0 from Chicago IBM Co., Armonk, NY) cleaned, coded and analyzed. Mean refractive measurements of the three devices in the two states of the eyes were compared using analysis of variance (ANOVA). Then the significant difference between instruments was ascertained with Post hoc test for in between instrument comparison using their mean differences. Mean non- cycloplegic and cycloplegic refractive measurements of the three devices of the study participants recruited were presented on tables side by side for all the instruments. For all comparisons done, the level of significance was put at p < 0.05.
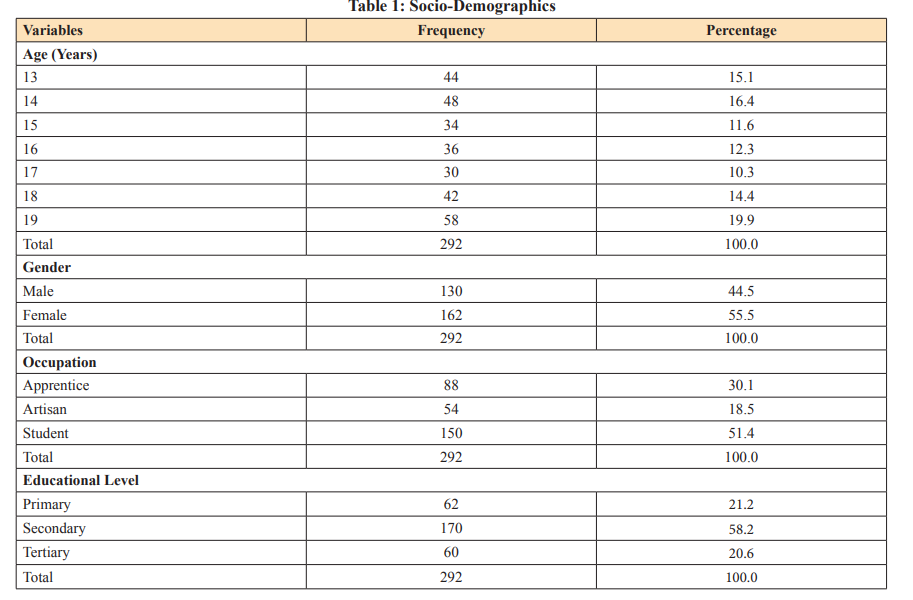
A total of two hundred and ninety- two adolescents (584 eyes) were enrolled into the study and had their refractive errors measured using Smartphone-based auto refractor, tabletop auto refractor and retinoscope under non-cycloplegic and cycloplegic states. The mean age of the study participants was 16.6+0.76years, (age range of 13-19years). They comprised of 162 (55.5%) females and 130(44.5%) males; giving a female to male ratio of 1.3:1. While those aged 19years constituted majority 58(19.9%) of the study participant, those aged 17year were the least 30 (10.3%) (Table1).
A total of 52(8.9%) eyes comprising {22(7.5%) right eyes and 30(10.3%) left eyes} had normal vision in an unaided visual acuity test despite having an improvement of one or more line with Pinhole test (Table2).Five hundred and thirty-two (91.1%) of the 584eyes studied had various degrees of uncorrected visual impairment (VI) according to WHO definition of visual impairment; ranging from mild VI: 114(19.5%), moderate VI: 340(58.2%) and severe VI: 78 (13.4%). With PH, about 80% achieved normal VA, 20% were between mild and moderate VA and there was none with severe VA (Table 2).

*Normal vision here refers to Log Mar VA of less or equal to 0.2 (6/9)2
In non-cycloplegic state, 430 (73.6%) eyes were found to have refractive errors. The mean spherical value of myopia and hyperopia measured by SPBAR and TTAR were significantly higher than that measured by retinoscopy. Also the mean spherical equivalent value of myopic astigmatism measured by SPBAR and TTAR showed no significant difference to that measured by retinoscopy. But the mean spherical equivalent value of hypermetropic astigmatism measured by SPBAR and TTAR were significantly lower than that measured by retinoscopy. The overall ranges of spherical values measured in non-cycloplegic state was -4.00Dto 5.38D while the range of spherical equivalent values measured in non-cycloplegic state was-10.75D to 5.38D, (Table 3).
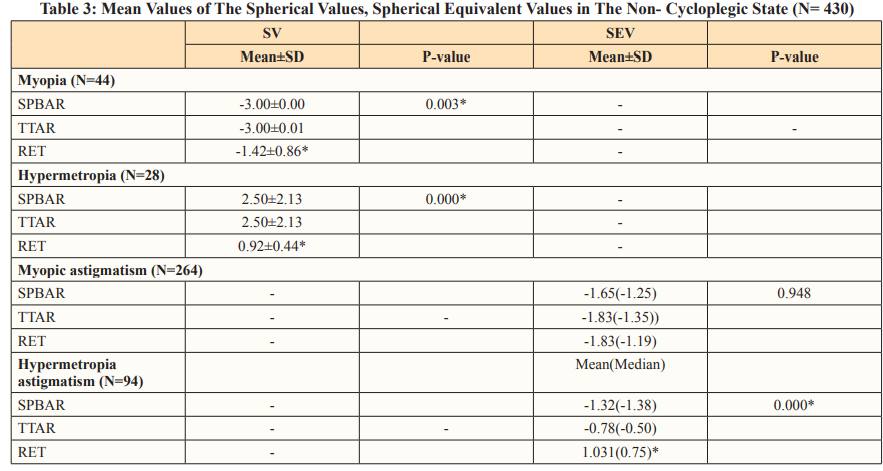
SPBAR= Smartphone-based auto refractor, TTAR=Tabletop auto refractor, RET= Retinoscopy *Significant P<0.05. For Myopic astigmatism and hypermetropia astigmatism, due to non-normality of distribution, Krukal Walli’s test (Non parametric test) was used to compare the values among the instruments of the study.
In cycloplegic state,461(78.9%) eyeswere found to have refractive errors following study definition(≥±0.50D); comprising 31(5.3%) myopia,30 (5.1%)hypermetropia, 320(54.8%) myopic astigmatism and 80(13.7%) hypermetropic astigmatism. The mean spherical value of myopia and hyperopia measured by SPBAR and TTAR were significantly higher than that measured by retinoscopy. Also the mean spherical equivalent value of myopic astigmatics as well as hypermetropic astigmatics measured by SPBAR and TTAR were significantly lower than that of retinoscopy. The overall range of spherical value measurement was -4.25D to 4.00D while that for spherical equivalent values was -10.75D to 4.50D for retinoscopy, (Table 4).
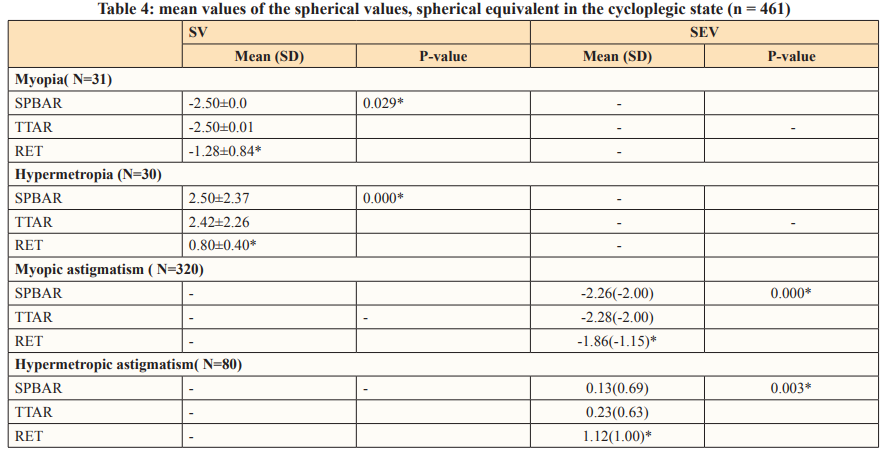
SPBAR=Smartphone- based auto refractor, TTAR= Tabletop auto refractor. RET = Retinoscopy
*Significant P<0.05. For Myopic astigmatism and hypermetropia astigmatism, due to non-normality of distribution, Krukal Walli’s test (None-parametric test)was used to compare the values among the instruments of the study.
In non- cycloplegic state, the mean spherical values (SV) measured by TTAR was significantly lower (p= 0.041) among older adolescents aged 15 to 19years than that of the younger adolescents aged 13 to 15 years but the measurements by SPBAR and Retinoscope showed no difference(p= 0.724 and 0.996 respectively ) in both age categories of the adolescents. The mean spherical equivalent values (SEV) measured by SPBAR, TTAR and Retinoscope did not show any significant difference (p= 0.825, 0.556 and 0.830 respectively) in both age categories of the adolescents (Table 5).
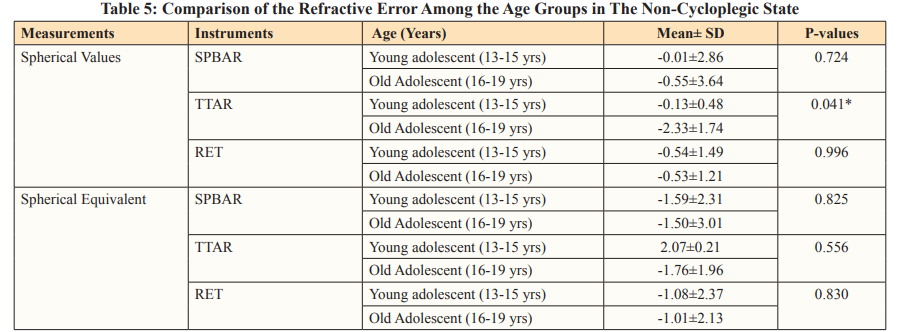
*significant P<0.05 Comparison using the Mann Whitney U-test
In cycloplegic state, the mean spherical values (SV) measured by SPBAR and TTAR were significantly lower (p= 0.028 and 0.005 respectively) among older adolescents aged 15 to 19years than that of the younger adolescents aged 13 to 15 years but the measurements by Retinoscope showed no difference ( p= 0.378) in both age categories of the adolescents. The mean spherical equivalent values (SEV) measured by SPBAR, TTAR and Retinoscope did not show any significant difference (p=0.638, 0.607 and 0.372 respectively) in both age categories of the adolescents, (Table 6).
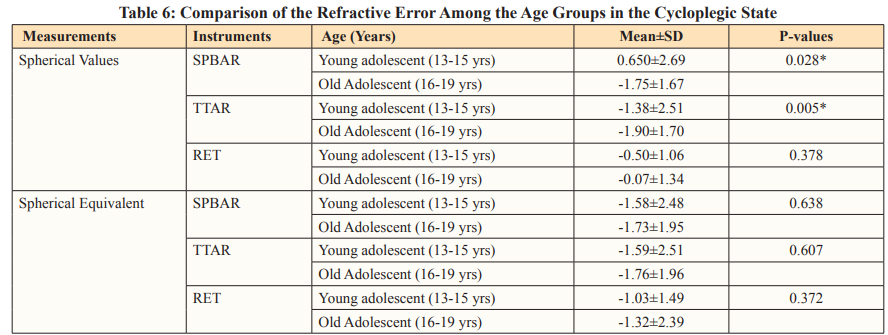
*significant P<0.05 Comparison using the Mann Whitney U-test
A total of 292 adolescents with refractive errors took part in the study and 584 eyes were assessed and analyzed. This is similar to the number of eyes assessed in the work of Malhotra et al [23]. They assessed 540 eyes of 270 Indian adolescents for refractive error. The socio-demographic data of this study participants showed that the mean age of the study participants was 16.6 +0.76 years with a range of 13 to 19 years implying that study participants were adolescents. This age range was narrowed in order to keep to WHO definition of adolescents; who are known to have high prevalence of refractive errors [7,24]. Moreover, this age range is in keeping with the age specifications of the study instrument (Smartphone -based auto refractor) [25]. The mean age was similar to that in some other studies published in 2016 among Indian adolescents and Children of Darfur Sudan respectively on refractive error prevalence in which refractive error prevalence was studied among adolescents aged 10 to 19 years and children aged 12 to 15 years respectively [23-25].
There were more females 162 (55.5%) than males 130(45.5%)in this study, giving a female to male ratio of 1.3:1. Kenneth et al in their study in 2015 which compared SV One handheld auto refractor with other auto refractors also had more females (52) than males (48). Another study by Shuyu et al published in 2017 which compared three auto refractors among Chinese adolescents with uncorrected refractive errors had more males 1048(50.6%) than females 1024(49.4%) [26,27]. There was no uniform pattern of gender distribution across studies. The major proportion 150 (51.4%) of the participants in the present study were students. Aina et al in their study in Ibadan Nigeria on refractive error amongst black adolescents aged 13-21years with mean age of 15.1 ± 1.9 years detected refractive errors in 41.3% of them who were all students using auto refractor. This further shows that the participants have pressing needs for detection and correction of their refractive error for effective performance in their studies [28]. The educational level also showed that 170 (58.2%) were at secondary school level and 60 (20.6%) at tertiary which buttress the need for good vision to excel in their various areas of endeavor.
The grouping of the refractive measurements of the three test instruments into Myopia and hypermetropia for spherical value (SV), myopic astigmatism and hypermetropic astigmatism for spherical equivalent values (SEV) was done using retinoscopy (the gold standard) as the reference. In this study, the Smartphone- based auto refractor compared closely to TTAR but not retinoscopy in non-cycloplegic state of the eyes both in measuring of SV and SEV. This is similar to the findings of Rotsos et al in their study who also noted that autorefractometer in children (in whom accommodation is more active than older patients) without cycloplegia could not measure upto Manual retinoscopy which is still the most accurate technique to estimate refractive status in children. Also in the work of Shuyu ng et al, it was found that the results of the three autorefractors used in the study were clinically acceptable in the children and adolescents aged 4 to 18 years and can be used interchangeably in a large-scale study or in screening for the detection of refractive error and determination of the prevalence rates of refractive errors; in keeping with the findings of this study.
In this study, the NETRA Smartphone-based auto refractor compared closely to tabletop auto refractor but not retinoscopy in cycoplegic state of the eyes in measuring of both SV and SEV. This is in keeping with findings of Agarwal et al in their study on Netra device which though is significantly less expensive, a viable and robust lower-budget option device for low income countries, it’s relatively less accurate when compared to manual retinoscopy. This is contrary to the work of Goktug Demirci et al which showed that cycloplegic autorefractometer and retinoscopy results are similar especially and a useful tool for estimating refraction in patients for whom conventional autorefraction is not an option.
Comparison of Refractive Measurement Values of Smartphone-Based Auto Refractor, Tabletop Auto Refractor and Retinoscopy in Non- Cycloplegic And Cycloplegic States Placing the results of Smartphone-based auto refractor and tabletop auto refractor side by side in both non-cyclpolegic and cycloplegic states in this study, it was found that Smartphone- based auto refractor have consistently compare closely with Tabletop auto refractor in measuring all types of refractive error in both cycloplegic state and non-cycloplegic states. Although the refractive values of tabletop auto refractor were slightly higher in cycloplegic state, The values of both SPBAR and TTAR were quite close and consistent across all refractive error types measured in non-cycloplegic state. The findings were similar to that of Yee Fong et al which was published in 2006 and compared three auto refractors with Subjective refraction in non-cycloplegic and cycloplegic states. However, these differences in both studies can be accounted for by the variations in their sample size of 117, age range of 7- 12years among the white populations as well as differences in their study technique and test instruments. The finding of this study which agrees to a reasonable extent to other studies. implies that Smartphone-based auto refractor can be valuable in measuring all types of refractive errors in non- cycloplegic and cycloplegic states [29,30].
The NETRA Smartphone-based auto refractor was found to be a reliable alternative to tabletop auto refractor both in non- cycloplegic and cycloplegic states in measuring refractive errors in adolescents. It is however, not yet a substitute for retinoscopy which is still the gold standard. Also, NETRA Smartphone auto refractor had similar outcomes with tabletop autorefractors in measuring spherical values (SV), and spherical equivalent values (SEV). However, though Smart phone does not measure up to the retinoscopy which is the gold standard, the refractive measurements were consistent in both non-cycloplegic and cycloplegic states; thus, may be effectively used to measure and diagnose refractive errors in busy ophthalmic clinics and refractive error screening programs [31-83].
