Author(s): Juan L Segura Masís*, Rodrigo Masís Mejías, Katherine Alfaro Navas, Santiago Rodríguez Picado, Juan L Segura Valverde*
69 patients have undergone hemispherectomy and temporal lobectomy since the creation of the UMCE in November 2000. Of these, 18 (26%) underwent hemispherectomy and 51 (74%) underwent temporary lobectomy. A sample of 31 patients (45%) were obtained, which met the inclusion criteria. The average age of initiation of treatment at the HNN was 5.5 years old (66 months) and the average age at which they underwent surgery was 10.8 years old (130 months). There was one patient in the sample who received 9 anticonvulsant medications before undergoing the surgical procedure and the average number of medications used pre-surgically was 4.45 anticovulsivants per patient. The average postoperative medication was 2.35 anticonvulsivants per patient. The average monthly preoperative cost was $50.17, while the postoperative period was $31.26, with a difference of $18.91. A total of 9 patients in the sample increased the monthly postoperative cost. The total savings per month in the patients included in the sample was $586.36 and extrapolated to the population of 69 patients resulting in a saving of $1,305.14 per month. The projection according to the life expectancy of the patients in the sample translates into a saving of $409,188.59 while the projection to the 69 patients would result in a saving of $910,774.60 for the Caja Costarricense del Seguro Social (CCSS - Costa Rican Social Security Fund).
A patient is said to be refractory to treatment with antiepileptic drugs (AEDs), when he has used at least two anticonvulsants with adequate indication and doses in monotherapy or polytherapy without reaching a crisis-free state [1,2].
Despite the continuous appearance of new anticonvulsant drugs, about 30% of patients with epilepsy are refractory to pharmacological treatment [3].
In the 80s, a current of thought began in the neurosurgical community, where it began to be observed that certain areas of the brain could be removed without having greater neurological involvement in the patient with brain disease, even if an entire hemisphere was removed or disconnected from its counterpart [4]. At the time, it was observed that patients with severe diseases, such as giant tumors and severe hemosiderosis, retained the motor function they had prior to surgery, which included the removal of a large portion of the brain invaded by the tumor or affected by hemosiderosis. Previously, it was also observed that these surgeries, where one or more brain lobes were removed, had very good results for patients with refractory epilepsies [5]. These and other studies served as a theoretical basis to start offering this therapeutic alternative to patients. With refractory epilepsy in Costa Rica, mainly for the pediatric population [5,6].
This unit, created in 2000, required a heavy investment by the CCSS Medical Management -, an office that authorized and directly assigned the funds, since it required the purchase of electroencephalogram video equipment, the payment of two technicians in said unit, availability payment for Neurology professionals and overtime for technicians.
The purpose of this research is to determine the cost of antiepileptic drugs for HNN and CCSS. This with regards to the care of patients undergoing surgical procedures, such as hemispherectomy and temporal lobectomy since these are the procedures with the best clinical results, for the treatment of epilepsy refractory to medical treatment. This before carrying out the procedure and comparing them with the costs of the subsequent control that they required [7,8]. This way, it can be established whether or not there was significant savings for the Institution. It was decided to choose these two groups of patients since they represent the most complex surgical procedures, they are the patients who use the greatest amount of epileptic drugs due to the severity of their seizures and the clinical results are more evident [7,8].
The results of this work will help the HNN and the CCSS to define the institutional policy regarding the specialized unit and funds that will make the program sustainable.
This study is retrospective, descriptive, quantitative and longitudinal, of the patients who underwent surgery for refractory epilepsy, specifically hemispherectomy and temporal lobectomy at the National Children’s Hospital of Costa Rica, in San José from November 2000 to December 31, 2018.
Patients classified as epileptics refractory to medical treatment and who underwent hemispherectomy or temporary lobectomy as an alternative treatment at HNN.
Statistical analysis: The data, tabulated in an Excel table, was used to establish monthly costs, calculate total costs, and calculate the pre and post-operative difference. For patients whose preoperative or postoperative control period was less than one year, this was adjusted to months for comparison purposes. The monthly average of costs in preoperative drugs provided by the Pharmacy Department of the HNN, were compared with the monthly average of costs of postoperative drugs. Subsequently, the current life expectancy in epileptic patients was projected, (according to the Spanish Society of Neurology is 10 years less than the life expectancy of people without the disease) and that in 2016 it was around 79 years in Costa Rica, resulting in an expectation of 69 years in the population sick (828 months) [9,10]. This result was used to project the total cost savings of anticonvulsant drugs that would be obtained over the life expectancy of these patients undergoing hemispherectomy and temporary lobectomies, in case of demonstrating savings for the CCSS. If the ratio of preoperative cost vs. postoperative cost is greater than 1, it implies that there is an economic benefit; if it is less than 1, it implies that there is no economic benefit; if it equals 1, it is indifferent.
The mean Z alpha method was used to determine the sample size and the Student’s T test was used to make the tests of significance for two related samples.
The cost of medicines for patients decreased on a monthly average from $50.17 to $31.26 resulting in a difference (saving) of $18.91 per month per patient, which means a 38% decrease in monthly average. For the patients in whom the suspension of all antiepileptic drugs was achieved, a cost of $ 0 was assumed until December 2018 for comparison purposes. With this data and with the average life span in which they were operated, it was projected what the institution would have saved at the end of this period with the people included in the sample and the population. Taking these figures as a reference, the total saving according to the life expectancy in the sample was calculated in $409,188.59 and in $910,774.60 counting all the people who have undergone a hemispherectomy or temporary lobectomy. The summary of these results is observed in (Table 1).
| Table 1: Results | |
|---|---|
| Population | 69 |
| Sample | 31 |
| Life expectancy in months | 828 |
| Preoperative monthly average cost | $50.17 |
| Postoperative monthly average cost | $31.26 |
| Difference of averages | %18.86 |
| Average age at the start of preoperative treatment (months) |
66 |
| Average age at the start of postoperative treatment (months) | 130 |
| Total savings per month in the 31 patients (sample) | $586.36 |
| Total savings per month in the 69 patients (population) |
$1289.34 |
| Average life expectancy of the 31 patients (months) | 698 |
| Total savings according to life expectancy of 31 patients |
$409,188.59 |
| Total savings according to the life expectancy of the population (69 patients) |
$910,774.60 |
When reviewing data, it can be seen that 9 patients increased the postoperative monthly cost and this was due to the fact that they used much more expensive medications, such as gabapentin. With these results and with the life expectancy of these patients, a projection was made where it was calculated how much it would cost the CCSS to finance the treatment of these people and thus infer the savings over time.
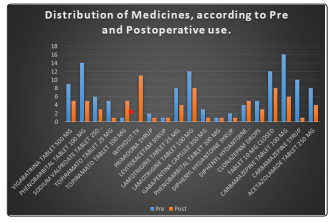
Also associated with the appearance of the medications, as observed in Figure 1, it was found that the most widely used medication was carbamazepine in a total of 26 patients, followed by valproate and lamotrigine in 20 patients. On the other hand, medications such as levetiracetam and phenobarbital were only used in one patient, respectively. This use of complex medications is due to the fact that the patients who are managed at the HNN are referred from other centers once they are classified as refractory epileptics. This means that they have most likely already tried to control their seizures with first-line drugs and, for this reason, newer and more expensive drugs should be used, which are only prescribed at the HNN for being a highly specialized center.
It is important to emphasize that in the management of postoperative patients, some used a greater number of medications than before their surgery, this in part because the care protocol consists of using previously prescribed medications again. It is considered safer to prescribe innocuous medications and subsequently decrease their dose until they are eliminated from the treatment scheme, so it is possible that some of these patients over time eliminated one, several, or all of the medications.
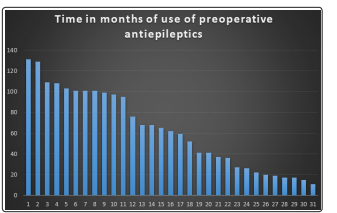
It was documented that all the patients, except one, had medication for more than one year, and even more than half of the patients had medication for more than 5 years. The average age of initiation of treatment in the HNN was 5.5 years old (66 months) and the average age at which they underwent surgery was 10.8 years old (130 months). This shows that some patients are late referred to higher levels of care. Associated with this, as seen in Table 5, there were patients who received up to 9 different medications before undergoing the surgical procedure, which causes increases in the patient’s waiting time, even exceeding 60 months (5 years), as seen in figure 2.
The effectiveness of surgical treatment for refractory epilepsy in the economic aspect could be evidenced in our study since a monthly saving was demonstrated that turned out to be significant when comparing the costs of medications used before and after hemispherectomy and temporary lobectomy surgeries, as well as significant savings for the health system both in the short and long term. Despite the above, it is necessary to improve the way in which patient information is stored, this because in this case it was impossible to carry out an investigation with more variables such as hospital stay, surgical time, among others. It is important to reinforce this aspect in order to be able to make a more accurate calculations of what is involved in the pre and post-surgery treatment of these patients in the future.
