Author(s): Rafael Ricci Ferrari Manéa, Rivadavio Antunes M. de Oliveira*, Gustavo Conrado Brassaroto, Eni Martins Medeiros and Stephanie Pedrazza
Introduction: Metastasis in the thyroid itself, is unusual, represents 1.5-7.5% of malignant thyroid lesions and the original site of the colon is rare, around 0.1% incidence. The objective is to report the case of a patient diagnosed with colorectal cancer which progressed to thyroid disease.
Case Report: It is a 62-year-old male patient who was being followed up at the Cancer Hospital of Londrina due to the resected colon neoplasm, which evolved with disease recurrence for the liver and lung and was controlled with systemic chemotherapy. It evolved with progression to thyroid and it was opted for diagnostic surgical resection.
Conclusion: In the case demonstrated, it is a rare presentation of colon cancer metastasis and there is no current literature which would be a better therapeutic approach; surgery or palliative systemic chemotherapy. In this scenario, the importance of reporting cases little described in the literature may help in the decision of future conduct.
Thyroid metastasis is unusual, represents only 1.5-7.5% of malignant lesions, and the most common primary sites are: kidney, lung and breast. The incidence of thyroid metastasis originating from the colon is rare, around 0.1% [1]. The objective is to report the case of a patient with colon cancer diagnosed in 2018 who was undergoing palliative treatment since 2020 and developed a thyroid nodule in 2022 with PAAF suggesting papillary thyroid carcinoma, but after thyroidectomy, a diagnosis of colorectal metastasis was made.
A 58-year-old male patient started with abdominal pain associated with episodes of hematochezia in August/2018, in this period he had worsening of abdominal pain and sought medical care in the emergency room. After medical evaluation, he was diagnosed with perforated acute abdomen and referred to emergency surgery. During the procedure, colon neoplasm was discovered and right colectomy was performed. The pathological diagnosis showed tubular adenocarcinoma consistent with colorectal origin, pT3N1 - EC IIIB, BRAF and wild-type RAS, with microsatellite stability. The first appointment with clinical oncology was in September/2018, but the patient had no clinical performance to start adjuvant chemotherapy due to surgical recovery. While awaiting clinical improvement, routine tomographies were requested, which showed liver and local recurrence. Subsequently, he was evaluated by oncological surgery and in March/2019 he was submitted to hepatic metastasectomy and resection of the local recidivist tumor.
After surgical procedure, “adjuvant” chemotherapy was indicated and performed the treatment with the FOLFOX scheme (5-FU+oxaliplatin) for 12 cycles - from March/19 to August/19. Five months later, new irresectable liver and pulmonary lesions appeared, characterized by disease progression and started firstline palliative treatment with FOLFIRI scheme (5-FU+ irinotecan).
In January/2022, the patient was being treated with FOLFIRI and maintained stable liver and pulmonary disease, when cervical nodular mass of 3x3 cm was found, painless associated with hoarseness (Figure 2). In June/2022, needle aspiration puncture was performed and cytological result compatible with category V of the Bethesda system and suspicious for papillary carcinoma of thyroid origin.
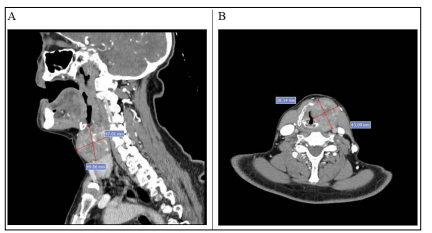
Figure 2: Neck tomography (A and B) shows expansive lesion in the left lamina of thyroid cartilage that extends to left thyroid muscles, left glottic, and para epiglottic space
Patient was referred and evaluated by the head and neck surgery team and in 07/22 underwent total laryngectomy, cervical emptying and thyroidectomy. The immunohistochemical result showed that it was metastatic colorectal cancer - CK7 and TTF-1 negative, CK20 and CDX2 positive (Figures 3A,B,C,D).
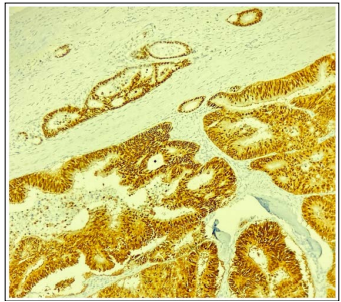
Figure 3 (A): CDX2 - Strong and diffuse nuclear expression in tumor cells

Figure 3 (B): HE - Complex glandular formation exhibiting atypical and depolarized nuclei, with extensive areas of necrosis
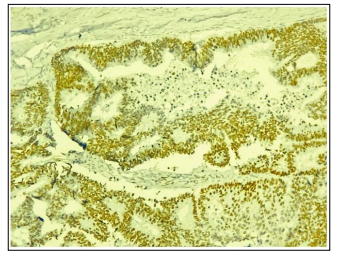
Figure 3 (C): SATB2 - diffuse nuclear expression in tumor cells
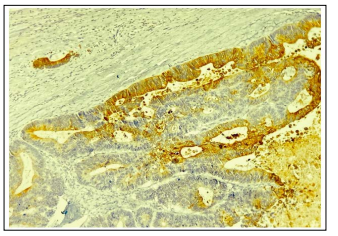
Figure 3 (D): CK20 - cytoplasmic expression in tumor cells
In the postoperative period, patient evolved with a severe infectious complication and died due to septic shock of pulmonary focus days later. Patient survival from the first recurrence to death was 43 months.
Colorectal cancer is the third most common in both sexes. In 2020, 1.9 million new cases were diagnosed and responsible for 935 cancer-related deaths. It is estimated that by 2035 the number of colon cancer-related deaths will increase by up to 60%. There are multiple risk factors for the development of the disease distributed in the following groups: related to previous and family history, lifestyle and others (Figure 1). The diagnosis is made with colonoscopy that is indicated for screening in risk groups or investigation of symptoms such as intestinal bleeding, abdominal pain and consumptive syndrome [2].
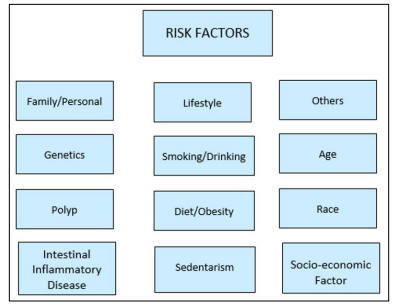
Figure 1: Risk factors in colorectal cancer
In the initial scenario, the curative treatment is based on surgery and the addition of adjuvant chemotherapy according to staging. Approximately 50-60% of colon cancer patients develop metastases and the most common site is the liver [3,4].
Primary thyroid neoplasm represents 1% of all cancers in the US. Ultrasound-guided fine needle puncture is the main diagnostic method and the basis of treatment is surgery. Secondary histology in this case is rare, especially in the case of colon and in this scenario there is a discussion of metastasectomy to bring benefit to global survival [5,6].
Metastasis to thyroid gland is unusual; authors suggest that this is due to the cellular microenvironment, rich in oxygen and iodine associated with a high blood flow, which hinders the growth, implantation and survival of neoplastic cells. In a series of autopsy, the most common primary thyroid metastasis sites were: pulmonary, renal, and gastrointestinal tract [7].
The main sites of colorectal cancer metastasis, excluding lymph nodes, are the liver and lung, through the hematogenic pathway through the portal circulation. The route until reaching the thyroid is uncertain, but data show that patients with thyroid metastasis may already have lung injury [8].
Symptoms related to thyroid metastasis are: appearance of a nodule in the neck, dysphagia, dysphonia and cough. Treatment may vary from surgery, radiotherapy or systemic chemotherapy, but there are few data in the literature on what the best conduct is [9].
In a study conducted at the Memorial Sloan Kettering Cancer Center, 8,410 cases of biopsies or thyroid surgical resection were analyzed with a diagnosis of malignancy, and of these, only 0.36% were of secondary origin. The mean age at diagnosis was 63 years, the proportion between men and women was similar; of the 28 cases of carcinoma only 5 had colorectal origin and median survival from diagnosis ranged from 12 to 39 months [10,11].
The impact of thyroidectomy in case of thyroid metastasis is unknown, without a randomized phase III study since it is a rare site to be affected. Liévre et al suggests that surgery should be performed in symptomatic cases and that conservative management does not alter overall survival in the advanced disease scenario. Malani et al suggest that chemotherapy has low penetration in thyroid tissue, which generates little response to systemic treatment, so thyroidectomy would control the disease locally avoiding local symptoms such as airway obstruction, in addition, due to thyroid metastasis being rare, there is the possibility of being another pathology, for example, a papillary carcinoma, that is, a new primary tumor [1,7,12,13].
Primary thyroid tumors are usually positive for CK7 and negative for CK20. And in the reported case, there was a clear contrast between follicular cells that expressed CK7, PAX8 and TTF1 and metastatic cells that were negative for these markers, but positive for CK20 and CDX2 [14].
In the reported case, it is observed that this is a patient with advanced disease, with controlled hepatic and pulmonary metastasis and that after 2 years had disease progression to thyroid. The interval between diagnosis of primary disease and thyroid metastasis was similar to that observed in other case series, the initial symptomatology was similar to that described in the literature and the therapeutic option was surgery, since the systemic disease was controlled and the first hypothesis was papillary thyroid carcinoma [15].
Colon cancer with thyroid metastasis is rare, with few reports in the literature and there are divergent data regarding the best conduct to be taken. There are still challenges in the diagnosis and a pathologist dedicated to the type of tumor in question is needed. The role of the surgeon is fundamental to the clinical outcome and seems to be associated with the control of local symptoms, but it is unclear whether metastasectomy can benefit overall survival.
I declare there is no conflict of interest in the reported case.
Informed consent of the family was obtained in writing for the publication of any potentially identifiable images or data included in the article.
