Author(s): <p>Makoto Akutsu, MD, PhD*, Yasuhiro Tsunemi, MD, Shota Saito, MD, Takashi Kashiwagi, MD, PhD, Tsuguhisa Nakayama, MD, PhD,<br /> Yasuhiro Tanaka, MD, PhD and Shin-ichi Haruna, MD, PhD</p>
Objective: To Analyze the time to treatment and visual prognosis of patients who presented with visual disturbance caused by sinus disease.
Methods: We retrospectively analyzed the post-surgery clinical course and visual acuity of 23 patients (24 sides) with rhinogenic visual disturbances from Dokkyo Medical University, Tochigi, Japan. Sinus diseases were classified into three groups: infection/inflammation (7 patients), mucocele (8 patients [9 sides]), and tumor (8 patients).
Results: Most patients (68%) were first admitted to the ophthalmology department and then referred to us. Patients with eye pain and ocular swelling were examined before those without symptoms (p < 0.05). In particular, the infection/inflammation group was more likely to present with symptoms other than vision loss and thus visit the rhinologists earlier. The infection/inflammation and mucocele groups showed improvement in visual acuity after surgery (p < 0.05).
Conclusions: Early consultation and surgical treatment were shown to be effective in the infection/inflammation and mucocele groups. For early rhinologist consultation, imaging studies should be performed for accurate diagnosis. Patients should be educated about the disease and encouraged to seek correct medical attention as early as possible.
Various lesions in the sinuses can, in severe cases, affect not only the sinuses but also the adjacent optic nerves and brain. Acute and chronic sinusitis generally present nasal symptoms such as nasal obstruction and rhinorrhea. On the other hand, acute visual disturbances due to rhinosinusitis are often accompanied by ocular symptoms, such as decreased vision and diplopia, without nasal symptoms. Past reports of sinus diseases resulting in acute visual disturbances can be classified into optic neuritis and optic neuropathy [1]. Visual disturbances may occur due to the invasion or compression of the optic nerve by a tumorous lesion [2].
Several studies have demonstrated an improvement in visual impairment after surgical treatment via nasal endoscopy for lesions in the paranasal sinuses. Surgical treatment includes controlling the infection by draining the abscess caused by an infection, opening the cyst if the cause is mucocele or pyocele, and removing pressure on the optic nerve by directly opening the medial orbital wall or the optic canal. However, the delay in detection and therapeutic intervention reduces the likelihood of vision improvement. Therefore, it is important to evaluate the cause of visual disturbance quickly and accurately. Although there have been case reports of improved vision, no reports have examined the efficacy of surgical treatment and visual prognosis across the three different pathologies of rhinogenic visual disturbances: infection/inflammation, mucocele, and tumor. Furthermore, there are currently no reports on the impact of time from onset to intervention in the different pathological conditions on visual prognosis. Therefore, we retrospectively examined the differences in clinical parameters, including visual prognosis, among rhinogenic visual disturbance cases classified by their causes (infection/inflammation, mucocele, or tumor).
Participants who were referred to Dokkyo Medical University with a primary complaint of acute visual disturbance, were diagnosed with rhinogenic visual disorders at our department, and underwent surgical treatment during the 10-year period from April 2011 to March 2021 were included in this study.
We referred to the medical records of patients who had undergone surgical treatment and evaluated the changes in visual acuity test results before and after treatment. We also collected information on the amount of time it took to receive surgery, the department that referred the patient, and the detailed location of the mainlesion on computed tomography (CT). Each patient’s consent was obtained verbally and in writing. This research was approved by the Ethics Committee of Dokkyo Medical University Hospital, and informed consent was obtained from every participant.
All visual acuity tests were performed at the Department of Ophthalmology. Visual acuity tests were performed preoperatively, 2 weeks postoperatively, and 3 months postoperatively. Additional visual acuity tests were added at other times as needed. In this study, we used the preoperative and 3-month postoperative evaluations. All but one patient underwent the Landolt ring test, which is widely used in Japan
Vision loss to the point of not being able to see the Landolt rings were described as “finger counting,” “hand motion,” “light perception,” and “no light perception,” and included evaluations that cannot be represented as decimal visual acuity. Decimal visual acuity was converted to the logarithmic minimum angle of resolution (logMAR) as follows: logMAR = log (1/decimal visual acuity). For those without values for “finger counting,” “hand motion,” “light perception,” and “no light perception,” the values were 1.85, 2.30, 2.80, and 2.90, respectively, based on previous studies [3].
CT was performed in all patients prior to the treatment intervention to investigate the cause of visual disturbances. CT was performed to determine if the orbit, optic nerve tract, and paranasal sinuses could be delineated. Images were constructed in axial, coronal, and sagittal sections in mediastinal (soft tissue) and bony conditions.
All surgical treatments were performed under general anesthesia using a nasal endoscope. In the infection/inflammation group, the abscess in the sinuses was drained. In cases where inflammation spread to the orbit and abscess was observed, the lamina papyracea was removed and the abscess in the orbit was drained. The mucocele group underwent surgery to open the cystic lesion. The cyst was opened as wide as possible, and the contents were removed and washed. In all cases, we confirmed no closed cysts remained using the navigation system. The tumor group was diagnosed based on surgical findings and a rapid pathological examination during surgery. Since the treatment plan was not fully determined at the time of the tumor diagnosis, the surgery included tissue collection and diagnosis. All surgical treatments were performed using a navigation system with CT images.
Statistical analyses were performed with SPSS version 28.0.0.0 (IBM, Armonk, NY). The Mann-Whitney U test was used to compare the two groups, and the Kruskal-Wallis and Bonferroni post hoc tests were used to compare the three groups. The changes in visual acuity before and after treatment were compared using the Wilcoxon signed-rank test. Statistical significance was established at p < 0.05.
We enrolled 23 patients who underwent surgical treatment during the study period and classified them according to the causative disease as follows: 7 cases of infection/inflammation (5 males, 2 females; Table 1), 8 cases of sinus mucocele (7 males, 1 female; Table 2), and 8 cases of tumor (4 males, 4 females; Table 3). One patient in the mucocele group simultaneously developed bilateral visual disturbance, resulting in a total sample size of 24 eyes.
The average age of onset was 38.8 ± 28.8 years for the infection/ inflammation group, 64.8 ± 9.4 years for the mucocele group, and 67.6 ± 8.6 years for the tumor group. Four cases in the infection/ inflammation group had onset in their teenage years, whereas no other disease showed such early onset.
The lesion site in the orbital region in the infection/inflammation group was subdivided using Chandler’s classification (Table 1) [4], with three cases (42%) classified as type I and four (57%) as type II.
All cases in the mucocele group had a history of previous sinus surgery via the sublabial approach (Table 2). The most common site of involvement was the posterior ethmoid sinus, especially Onodi cells.
Ophthalmology was the most common initially consulted medical department (15 cases [68%]), followed by otorhinolaryngology, neurosurgery, and pediatrics.
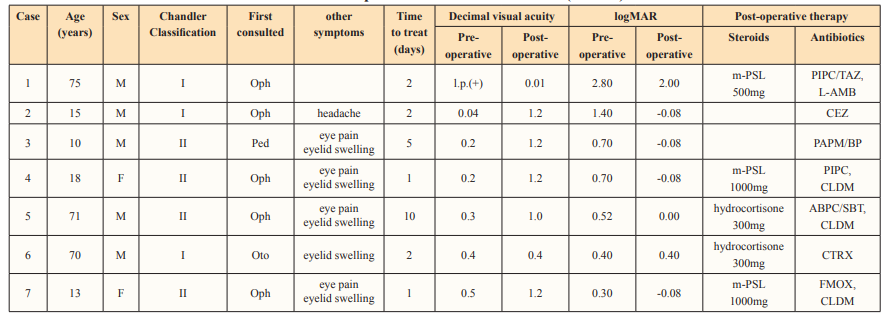
Op, ophthalmology; Oto, otorhinolaryngology; Ped, pediatrics; l.p., light perception; m-PSL, methylprednisolone; CEZ, cefazolin; CTRX, ceftriaxone; PIPC, piperacillin; CLDM, clindamycin; FMOX, flomoxef; ABPC/SBT, sulbactam/ampicillin; PAPM/BP, panipenem/betamipron; TAZ/PIPC, tazobactam/piperacillin.
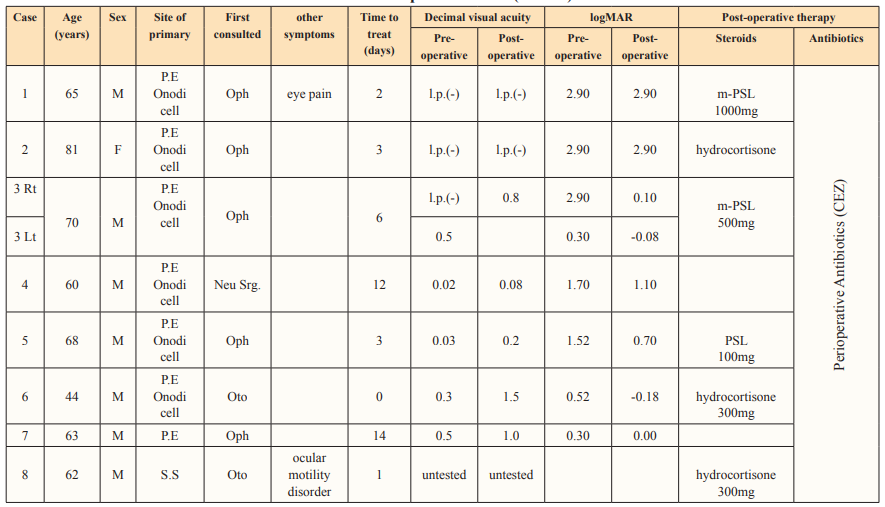
P.E., posterior ethmoid sinus; S.S., sphenoid sinus; Oph, ophthalmology; Oto, otorhinolaryngology; Neu Srg, neurosurgery;.p., light perception; PSL, prednisolone; m-PSL, methylprednisolone; CEZ, cefazolin
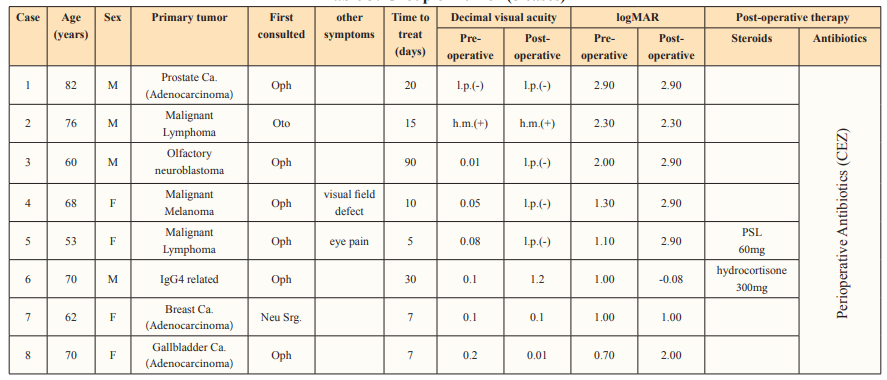
Oph, ophthalmology; Oto, otorhinolaryngology; Neu Srg, neurosurgery; l.p., light perception; h.m., hand motion; Ca., cancer; PSL, prednisolone; CEZ, cefazolin; CTRX, ceftriaxon
P.E : posterior ethmoid sinus, S.S : sphenoid sinus, Oph : ophthalmology, Oto : otorhinolaryngology, Neu Srg. : neurosurgery, Ped : pediatrics, l.p. : light perception, h.m. : hand motion, Ca. : cancer, PSL : predonisolone, m-PSL : methylpredonisoloneCEZ : cefazolin, CTRX : ceftriaxone, PIPC : piperacillin, CLDM : clindamycin, FMOX : flomoxef, ABPC/SBT : Sulbactam/Ampicillin, PAPM/BP: Panipenem/Betamipron, TAZ/PIPC : Tazobactam/Piperacillin
The average time required for consultation and treatment was 10.5 ± 17.9 days (3.2 ± 3.0 days for infection/inflammation, 5.2 ± 4.5 days for mucocele patients, and 23 ± 26.4 days for patients with tumor) (Figure 1A). The tumor group took significantly longer to see an otorhinolaryngologist than the other two groups (p < 0.01).
Figure 1B shows a comparison of the time taken to see the doctor between patients with only visual disturbance compared to those with other symptoms (not including nasal symptoms). Patients who reported visual disturbances took significantly longer than other patients (15.4 ± 22.1 days vs. 3.9 ± 3.3 days, respectively) to see a doctor (p < 0.05).
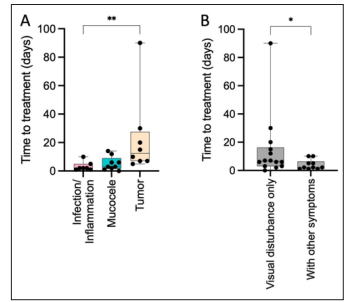
Figure 1: Time required to receive a medical examination. A. The tumor group took longer to see a doctor than the infection/ inflammation group (**p < 0.01). B. The group with only visual disturbances took more time to see the appropriate specialist (*p < 0.05).
Figure 2 shows visual acuity before and after treatment. Six patients (85.7%) in the infection/inflammation group and five patients (six sides) (66.6%) in the mucocele group had improved vision. These two groups showed a significant difference in visual acuity improvement with surgical treatment (p < 0.05). In contrast, only one patient in the tumor group (IgG4-related tumor classified as benign) had improved vision. The other seven patients were treated with chemotherapy, radiation therapy, and other anti-tumor treatments after the histological diagnosis, but their vision did not improve. Four patients (50%) displayed reduced visual acuity
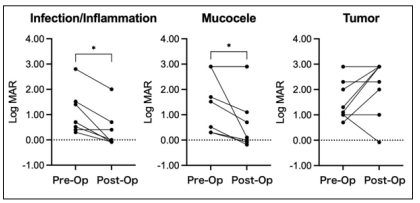
Figure 2: Changes in visual acuity test results before and after surgery. Surgical treatment significantly improved visual acuity in the infection/inflammation and mucocele groups (*p < 0.05). In the tumor group, visual acuity worsened in most cases.
Figure 3 presents the comparison of postoperative visual acuity improvement among the three groups. There was a trend toward better visual acuity in the infection/inflammation and mucocele groups compared to the tumor group, with a significant difference in the degree of improvement between the infection/inflammation and tumor groups (p < 0.05). In the infection/inflammation and mucocele groups, postoperative treatment included additional antibiotics and steroids without significant differences in drug use or visual prognosis between groups.

Figure 3: Evaluation of visual acuity improvement by surgical treatment. The infection/inflammation group had a significantly higher rate of visual acuity improvement than the tumor group (*p < 0.05).
In general, the causes of acute vision loss can be divided into three major categories: intraocular abnormalities (central retinal artery occlusion, retinal detachment, etc.), extraocular (optic nerve) abnormalities (optic neuritis/ neuropathy), and brain abnormalities (brain tumors, stroke, etc.). Although rare in Japan, traumatic eye injury, ocular hemorrhage and ophthalmorrhea, damage to the optic tract and optic nerve, and traumatic brain injury are also considered possible causes [5,6]. In this study, we focused on acute vision loss caused by nasal sinus disease.
Causes of rhinogenic visual disturbance can be classified into three categories: infection/inflammation in the sinuses directly or indirectly affecting the optic nerve, mucous cyst of the ethmoid sinus (especially the posterior ethmoidal sinus) and sphenoid sinus pressing on the optic nerve, and tumoral lesions in the orbit or sinus cavities invading and compressing the optic nerve [1,2].
Since rhinogenic visual disturbance is caused by a lesion in the sinus cavity, both nasal (nasal obstruction and rhinorrhea) and ocular symptoms (eye pain, swelling of the eyes and eyelids, and diplopia) will be observed in addition to vision loss. In the present study, none of the patients had nasal symptoms, while many presented ocular symptoms other than vision loss, explaining their selection of ophthalmology as the first department to consult.
In this study, we showed that surgical treatment can improve vision in patients with rhinogenic visual disturbance caused by either infection/inflammation or mucocele, which is consistent with other reports [7]. As such, early surgical treatment (especially within the first 24 h) can improve vision even in cases of severe vision loss [7]. The time from onset to surgery is also a predictor of postoperative visual acuity [8]. However, other studies report visual acuity improvement when treatment is provided within 6months of onset [9]. In our study, some patients had improved vision with surgical treatment 2 weeks after the onset of symptoms, while others who received treatment 3 days after onset did not. While early surgical treatment is undoubtedly desirable, we suspect that early treatment is not the only factor affecting postoperative visual acuity.
In the present study, two cases of mucocele were treated with surgery but still had vision loss. The optic nerve is recognized as one of the cranial nerves, but histologically it is considered part of the central nervous system. In peripheral nerve damage, Schwann cells are responsible for regeneration. However, since there are no Schwann cells in the optic nerve, once damaged, the possibility of regeneration is thought to be low. In addition, retinal microglia are activated by optic nerve damage and produce inflammatory cytokines, chemokines, and reactive oxygen species. These factors are thought to cause the accumulation of inflammatory substances in the optic nerve, which eventually leads to permanent vision loss [6]. Prolonged pressure from the mucocele is thought to cause thinning of the bone and direct pressure on the optic nerve, resulting in impaired blood flow [10]. In these two cases, the optic nerve was completely necrotic due to severe neuropathy caused by an inflammatory substance, combined with impaired blood flow, and it was assumed that the visual acuity did not improve even after the surgery.
In this study, visual disturbances in patients with tumor invasion were not improved by therapeutic intervention. Metastatic orbital tumors are often caused by metastases from breast cancer or malignant melanoma [11], while in our case, they were caused by metastases from a variety of primary tumors and nasal cavity cancers. It is almost impossible to differentiate between tumors using imaging alone, and a definitive diagnosis by lesions, tissue sampling, and pathological diagnosis is essential. We believe that early tissue sampling and histopathological diagnosis are important for early therapeutic intervention.
In this study, we summarized the causes of rhinogenic visual disturbances, the time required to consult a doctor, and visual prognosis after treatment. Although early surgical treatment is preferable, the present study shows that improvement may be possible even without early treatment. For early intervention, it is essential for the clinician who examined the patient at the initial visit to accurately assess the cause of disturbances through imaging and ophthalmologic studies. To achieve this goal, collaboration is necessary among ophthalmology and other departments where patients receive their initial consultation. Since residual visual disturbance has a significant negative impact on quality of life, it is crucial to proceed with appropriate treatment.
Acknowledgments: We would like to thank Editage (www. editage.com) for English language editing
Data availability statement: No additional data are available.
Funding: None
Conflicts of interest: There were no conflicts of interest in this study.
Authors’ contributions: MA: conception and design of the work, drafting, data analysis, interpretation of data, revising, final approval, agreement to be accountable for all aspects. YTsu: conception and design of the work, revising, final approval, agreement to be accountable for all aspects. SS: conception and design of the work, revising, final approval, agreement to be accountable for all aspects. TK: conception and design of the work, revising, final approval, agreement to be accountable for all aspects. TN: revising, final approval, agreement to be accountable for all aspects. YTan: revising, final approval, agreement to be accountable for all aspects. SH: conception and design of the work, drafting, revising, final approval, agreement to be accountable for all aspects.
