Author(s): Govathi Nikhila K*, Sushila Kataria, Yathin Mehata, Vikas Deswal and Manish kumar Singh
Coronavirus disease 2019 (COVID-19) is defined as illness caused by novel coronavirus now called severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2; formally called 2019-nCov), which was first identified amid an outbreak of respiratory illness cases in Wuhan City, Hubei Province, China [1]. A 3months Prior to the December 31st 2020 WHO was received a report of 9 cases of human who as being infected with novel coronavirus [1,2]. Later, on January 30, 2020 the WHO declared the COVID-19 Outbreak a global health emergency and on March 11, 2020 again they declared COVID-19 as global pandemic, its first such destination since declaring H1N1 influenza a pandemic in 2009. Further, more in February 11, 2020 the coronavirus study group of international committee of Taxonomy of viruses issued a statement announcing an official designation for the novel virus: severe Acute Respiratory Syndrome Coronavirus2 (SARS-CoV-2) [1]. Till date that is May 1st 2020 the whole world is still fighting against with this invisible enemy called “Coronavirus-COVID-19”. However still the vaccine is in trial.
Background: Coronavirus disease 2019 (COVID-19) is defined as illness caused by novel coronavirus now called severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2; formally called 2019-nCov), which was first identified amid an outbreak of respiratory illness cases in Wuhan City, Hubei Province, China [1]. A 3months Prior to the December 31st 2020 WHO was received a report of 9 cases of human who as being infected with novel coronavirus [1,2]. Later, on January 30, 2020 the WHO declared the COVID-19 Outbreak a global health emergency and on March 11, 2020 again they declared COVID-19 as global pandemic, its first such destination since declaring H1N1 influenza a pandemic in 2009. Further, more in February 11, 2020 the coronavirus study group of international committee of Taxonomy of viruses issued a statement announcing an official designation for the novel virus: severe Acute Respiratory Syndrome Coronavirus2 (SARSCoV-2) [1]. Till date that is May 1st 2020 the whole world is still fighting against with this invisible enemy called ?CoronavirusCOVID-19?. However still the vaccine is in trial.
Coronavirus: Coronaviruses are group of related RNA Viruses that cause diseases in Mammals and birds. In Humans this Viruses cause Respiratory tract infections that can range from Mild to severe [3]. It is highly contagious, It occurs through Human to Human transmission with approximately 2-10 days prior to individual becoming symptomatic [4,5]. It get transmitted through secretions, large droplets of cough, sneezing or running nose land on surfaces within two meters of infected person. So it is very important to maintain a physical distance of two meter while communicating. The virus can last for at least 24 hours on hard surfaces and up to eight hours on soft surfaces. It can also get transmitted by touching, eyes, nose, ears [6]. According many authors and researches till date the symptoms are Fever, cold and cough some times it is also a symptomatic. This infection Can starts with mild flue like symptoms or no symptoms and further progress to severe symptoms with an incubation period of 10-14 days. some primary symptoms to look for in COVID 19 Infected person are fever .dizziness,breathlessness,headache,dry cough , loss of smell and taste in some cases and also diarrhoea and fatigue [7].
Another important aspect which get effect due to this COVID-19 is the body system, majorly the Lungs. Severity of the COVID-19 infection depends on the effect of Respiratory function. If the COVID-19 Infection is severe then it has direct correlation with Acute Respiratory Distress Syndrome (ARDS). It may cause dry cough, heavy breathing, shortness of breathing, and increased heart rate. In most healthy individuals ,who do not have underlying issues COVID-19 exhibits mild symptoms which can be treated with medications and eventually patients get recover. In cases with severe infection may have impaired/low immunity levels due to underlying health conditions, may progress to severe ARDS, it eventually leads to pneumonia. The severity of COVID-19 has being divided into four categories.
First Category: These individuals are infected by the virus, but act as carriers but may not exhibit the symptoms. These individuals are at a higher risk of spreading the virus as they might be oblivious to its presence.
Second Category: Individuals with Mild fever, cough, headache or possible conjunctivitis. This is due to an infection in the upper respiratory tract.
Third Category: Similar to the third category, the symptoms here are more pronounced and might require hospitalization. Immediate treatment can help alleviate the symptoms and prevent a fatality.
Fourth Category: Severe cases of COVID-19, might lead to ARDS and Pneumonia. At this stage it is fatal [7].
Due to this Respiratory illness patient has difficulty in managing their breathing co-ordination. This improper co-ordination sometimes will effect the patients timing while swallowing the food or liquids which may further lead to Aspiration and Pneumonia if not diagnosed timely. So that is how it is very important to identify and manage the swallowing abilities timely in patients with Respiratory illness
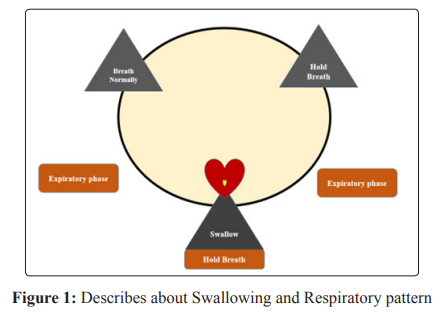
The following figure is Simplified description of the usual swallowing pattern in healthy adults. Swallowing initiates during the expiratory phase of the breathing cycle. Swallowing interrupts exhalation (swallow apnea), and once the swallow has been completed, breathing resumes with exhalation.
In people with Respiratory illness often have trouble with this timing. The airway closing during swallowing is called an apneic period. During a whole meal, there are hundreds of these apneic periods. Sometimes, when people have lung disease, this causes increase shortness of breath and fatigue. This fatigue may result in poor timing between respirations and swallowing. Sometimes, a person with acute respiratory illness/COPD or Lung disease may inhale vs. exhale after the swallow which causes penetration or ?aspiration? of food or liquid into the trachea (the tube to the lungs) or the larynx (voice box). This is can cause an ?Aspiration Pneumonia [8]. Sometimes swallowing may takes place with pain that is known as Odynophagia. The pain may be felt in mouth/ throat and can occur with or without difficulty in swallowing. This symptoms may range from a dull retrosternal ache on swallowing to a stabbing pain with radiation to the back so severe that patients cannot eat or even swallow their own saliva. Odynophagia usually reflects a severe inflammatory process that involves the oesophageal mucosa or in rare instances, the oesophageal muscle. The most common cause of Odynophagia include caustic ingestion, pill-induced oesophagitis, radition injury, and infectious oesophagitis.In these diseases, dysphagia also may be present, but pain is the dominant complaint [9].
Psychologically each and every person has being disturbed due to this COVID-19 pandemic throughout the world. However if we see about the patients with COVID-19 might be psychologically disturbed a lot then Normal. Once the patient hears about their positive result it may disturb their mental health and feel worried, anxiety or fear that are strong enough to interfere with one’s quality of life. For example if you take anxiety, the patient might be stressed, depressed, or may get panic attack which may disturb their life along with their family members. However, still there was no studies talking on these factors which made me interest to aim about this study
Aim: The Aim of the research is to sight the Chareteristics of Dysphagia in association with Odynophagia and to Point the Anxiety Levels of patients with COVID-19.
1. To sight the Characteristics of Dysphagia in association with Odynophagia.
2. To Point the Anxiety levels in COVID-19.
All patients who visited Medanta for First Screening were included.
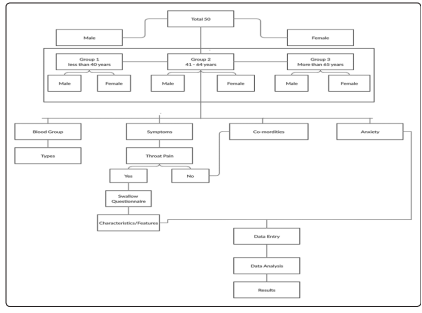
Overall first 50 positive COVID-19 patients were involved in this study in which firstly they all were divided according to their Age and Gender.
Secondly all this 50 patients were divided into Three Groups based on their Age factor I,e, Group-1 - Less than 40 years , Group 2 -41- 64 years and Group-3 More than 65 Years. Later on these three groups were further sub-divided, accordingly with their Gender.
All 50 COVID 19 patients were categorised accordingly with their Blood groups, Symptoms, Co-morbidities and Anxiety levels.
In these patients who has Throat pain as a symptom were categorised separately and dysphagia interview questionnaire was administered with those patients either through self/ telephonic audio /video consultation and the results were entered in google sheet.
All these patients were assessed with their Anxiety levels by using Hamilton Anxiety scoring scale.
A google sheet was developed with these scales and all results were marked accordingly to the patients feedback.
Patient and family concern was taken and also maintained the data confidentiality
Later on all scores were entered in excel sheet for further data analysis to elicit the results.
A total number of 50 Covid-19 positive patients were enrolled in the study from April to May 2020.The mean age of the patients was 53.2±20.0 (Range: 18 - 78) years. Among these, Males were 27 (54.0%) and females were 23 (46.0%) and the mean age of the male patients was 55.1±21.0 (Range: 18 - 78) years and females patients was 51.0±19.0 (Range: 22 - 77) years. Later on Patients were categorized in three age groups namely Group 1 (< 40 years), Group 2 (41 - 65 years) and Group 3 (> 65 years). Majority of patients were from Group 3 - 22 (40.0%) followed by Group 1 - 16 (32.0%) and 12 (24.0%) patients in Group 2. There was no significant difference observed in gender across the groups. Male: Female ratio was 1:1, 1:1 and 1.4:1 in Group 1, 2 and 3 respectively
In All 50 (100%) COVID-19 cases there are 22(44.0%) with A+VE blood group in which 7 (25.9%) were males and 15 (65.2%) were females, 17(34.0%) with B+VE blood group in which 13 (48.1%) males and 4 (17.4%) females, 3 (6.0%) with AB+VE blood group in which all were males with 3 ( 11.1%) and 8 (16.0%) with O+VE blood group in which 4(14.8%) males and 4(17.4%) were females.
Through this data we could see that mostly A+VE patients are more effected when comparing with other Blood groups and females are more than males with A+VE blood group.
Further, Fever and cold was reported most common symptoms in 32(64.0%) patients respectively (Fever:- Male - 55.6% & Female - 73.9%; Cold:- Male - 66.7% & Female - 60.9%) followed by weakness in 16 (32.0%) (Male - 37.0% & Female - 26.1%), Throat pain in 14 (28.0%) (Male - 25.9% & Female - 30.4%), cough in 12 (24.0%) (Male - 22.2% & Female - 26.1%), headache in 10 (20.0%) (Male - 11.1% & Female - 30.4%), breathing difficulty in 7 (14.0%) (Male - 18.5% & Female - 8.7%) and sneezing in 4 (8.0%) (Male - 7.4% & Female - 8.7%).
Hypertension was most common comorbidity in 21 (42.0%), diabetics was present in 13 (26.0%) and dyslipidaemia in 3 (6.0%) COVID-19 patients. History of respiratory illness and pneumonia were present in 8 (16.0%) and 6(12.0%) patients respectively. Out of 50 Covid19 patients there are 29 (58.0%) patients who are accepting Normal diet, 15(30.0%) accepting soft diet, 3(6.0%) are on Ryle’s tube Feeding and 3(6.0%) are on Ryle’s tube Feeding + Tracheostomy Tube.
All these 50(100%) cases with their symptoms divided accordingly with their age groups in order to see whether there is any significant difference present in relation with their age and symptoms and also to see which age group people more effected with common symptoms.
There are 8 (50%) with fever, 8 (50%) with cold, 8 (50%) with headache, 4 (25%) with cough, 2 (12.5%) with weakness, 6 (37.5 %) with throat pain and there are 3 (18.8%) cases with no symptoms. There is 1 (6.3%) patient with Hypertension present There is no Co-morbidities seen in this Group. Over all in patients with < 40 years age fever and cold and weakness are the most common symptoms and they don’t have any breathing difficulty, nor any history of respiratory illness or pneumonia .Among these 11(68.8%) patients were on Normal Diet and Graded with Swallow Level-7 based on National Outcomes Measurement Scale (NOMS) and 5 (31.3%) were on Soft Diet. Diet and Graded with Swallow Level-6 based on National Outcomes Measurement Scale(NOMS). All patients were Accepting orally , there is no patient dependent on tube feeding.
There are 8(66%) with fever, 10(83.3%) with cold,1(8.3%) with breathing difficulty, 1(8.3% ) with sneezing,4(33.3%) with weakness,1(8.3 %) with throat pain and there is 1 (8.3%) cases with no symptoms. Over all in this Group-2 with middle to old age i.e., from 41-64 years the breathing difficulty was present and started at this age range and there are 2(16.7%) patients with Diabetic, 1(8.3%) with Dyslipidaemia, 4(33.3%) with Hypertension , 2(16.7% ) with history of respiratory illness present and 2( 16.7%) with history of pneumonia were present in this group-2.Among these 8(66.7%) patients were on Normal Diet and Graded with Swallow Level-7 based on National Outcomes Measurement Scale(NOMS) and 2(16.7%) were on Soft Diet and Graded with Swallow Level-6 based on National Outcomes Measurement Scale(NOMS) and 1(8.3%) was on Ryle’s tube Feeding and 1(8.3%) was also on Ryle’s tube Feeding + Tracheotomised and these both patients were Graded with Swallow Level-1 based on National Outcomes Measurement Scale(NOMS) . According to the data if we see as the age increases the symptoms of Breathing difficulty was present and if it is associated with the history of respiratory illness or Pneumonia then the patients are at great risk and also on Tube dependent for feeding.
There are 16(72.7%) with fever, 14(63.6%) with cold,2(9.1%) with headache, 8(36.4%) with cough , 6(27.3%) with breathing difficulty, 3(13.6% ) with sneezing,10(45.5%) with weakness,7(31.8 %) with throat pain and there is 1 (4.5%) cases with no symptoms. Over all in this Group 3 , Old age group I,e >65 years patient has increased with breathing difficulty symptom along with Weakness due to which they are compromising with their immunity system, and there are 11(50%) patients with Diabetic, 2(9.1%) with Dyslipidaemia, 16(72.7%) with Hypertension , 6(27.3% ) with history of respiratory illness present and 4(18.2%) with history of pneumonia were present in this group-3.Among these 10(45.5%) patients were on Normal Diet and Graded with Swallow Level-7 based on National Outcomes Measurement Scale(NOMS) and 8(36.4%) were on Soft Diet Diet and Graded with Swallow Level-6 based on National Outcomes Measurement Scale(NOMS) and 2(9.1%) was on Ryle’s tube Feeding and 2(9.1%) was also on Ryle’s tube Feeding + Tracheotomised and these both patients were Graded with Swallow Level-1 based on National Outcomes Measurement Scale(NOMS) . According to the data if we seeas the age increases the symptoms of Breathing difficulty and weakness of the body were increasing and present in this age group patients .Due to low immunity system at this age it is difficult to the patient to fight against with this virus. These age group patients are at high risk to fight against with virus as they have low immunity system and if it is associated with the history of respiratory illness or Pneumonia then the patients are at great risk and also on Tube dependent for feeding some may also require Ventilation support. Overall, if we see as the age increases the severity of the problem increases despite of gender difference. Due to their low immunity control and symptoms and associated co-morbidities the Group-3(>65 years) people are at great risk and tube dependent when comparing to other two groups.
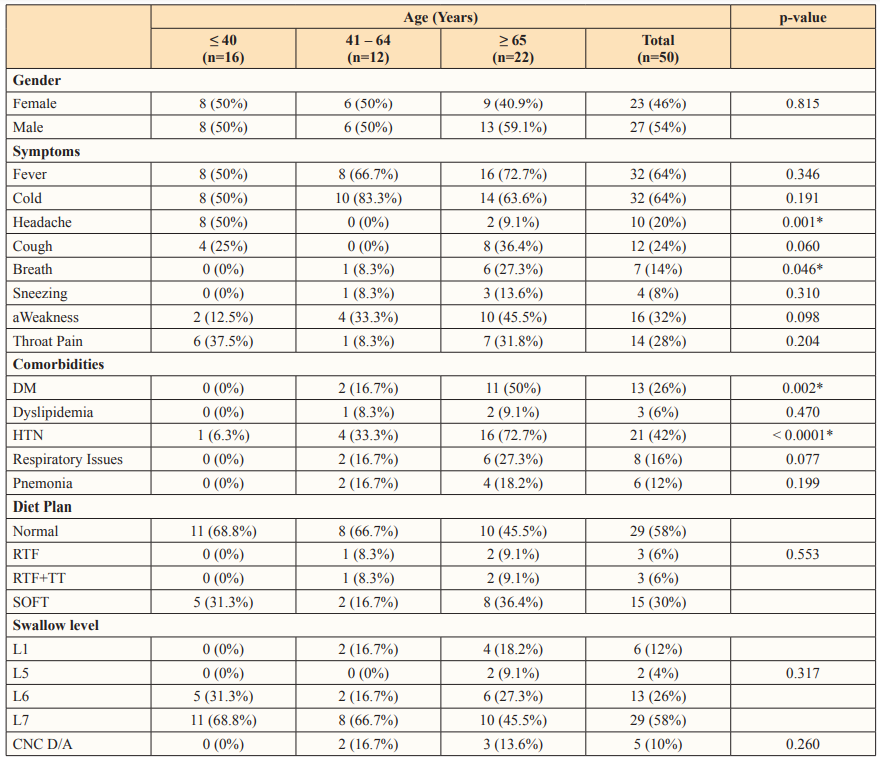
*p-value < 0.05, statistically significant.
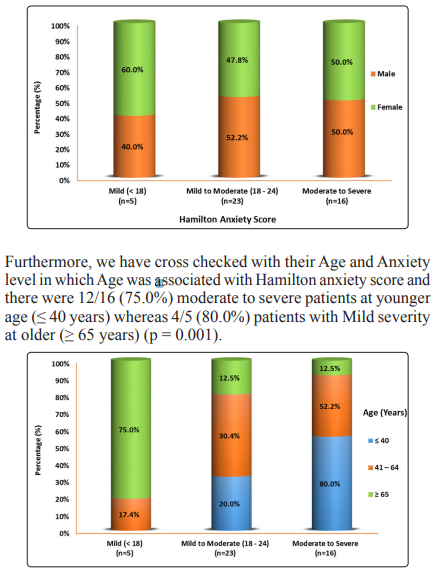
Out of 50 COVID-1919 patients, 44 were assessed with their Anxiety levels by using Hamilton Anxiety scoring (HAS) scale and 6 were not assessed due to clinical condition. The mean HAS score was 22.9±3.8 (range: 16 - 30). Patients Hamilton Anxiety score were categorized as mild (< 18), mild to moderate (18 - 24) and moderate to severe (25 - 30) categories. Among these 50 Covid19 patients there are 5 (11.4%) patients under Mild Severity, 23 (52.3%) patients with Mild to Moderate Severity and 16 (36.4%) patients under moderate to severe severity respectively. There was no association observed in gender in relation to their Anxiety categories (p = 0.885).
Later on, among all these 50(100%) COVID -19 cases there are 14(28.0%) patients presented with a Throat pain symptom and all were interviewed with Swallow Difficulty Questionnaire in order to check the characteristics of swallowing due to Odynophagia in patients with COVID-19. Among these 14(28.0%) patients 2(4.0%) were not interviewed because they are in Group -2 and on Ryle’s tube Feeding .Only the patients who are fully alert and conscious enough to participate in the study and primarily have a symptom of Throat pain where selected and interviewed.
A google sheet was developed to collect the information and for documentation purpose. All these 12(24.0%) patients were interviewed either through Tele-video consultation and some people were directly marked by themselves by sharing the goggle sheet. The swallow Difficulty Questionnaire consists of 14 questions in which patient gave with an option to choose either Yes or No. After collecting and completing the goggle sheet from all the 12 (24.0%) patients with throat pain where categorized and divided into two groups namely ? 60 years and > 60 years along with their gender difference .Finally, among these 12(24.0%) patients there are 7(58.3%) male and 5(41.7%) female. There are 7(58.3%) with ? 60 years of age group and 5(41.7%) with >60 years of age group. Among these 12 (24.0%) patients there are 11(91.7%) patients who are taking soft Diet and 1(8.3%) patient who is on Normal Diet. The below table shows about the characteristics of swallowing difficulty in relation with odynophagia in COVID-19 Patients.
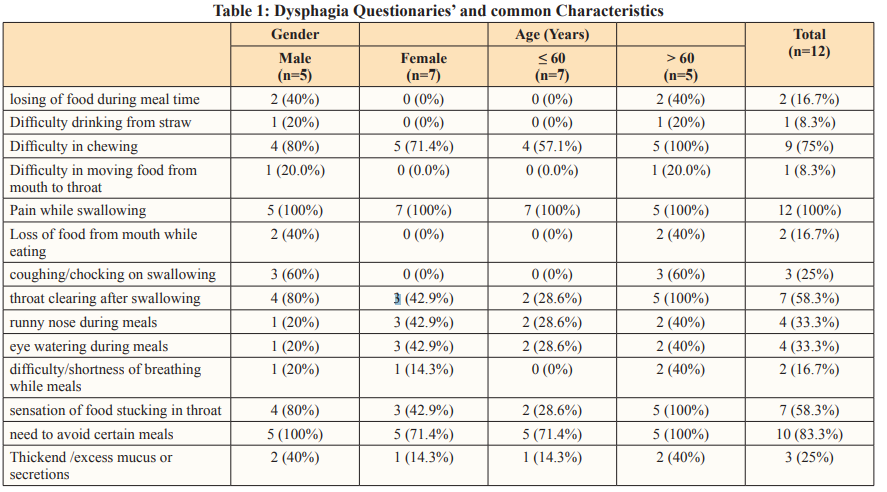
It is very less number in order to conclude anything .However, we need a large sample study and this study is still going on to have a better standard results to check the co-relations and characteristics. But as of now with this current data it shows that patients have few common characteristics like Pain while swallowing, Difficulty in Chewing, Need to avoid certain meals due to pain, throat clearing after swallowing as a common most characteristics of Dysphagia in Relation with Odynophagia in patients with COVID-19.
Conclusion: However, we need a large sample study in order to standardise any dysphagia characteristics and we are still working on this study. This study also concludes that the Younger patients
has Moderate to severe Anxiety level when compared with to the Old age group despite of their symptoms and gender difference and hence it is statistically significant with p-value 0.0001.
