Author(s): Ayse Gul Kocak Altintas
Central serous chorioretinopathy (CSCR) is characterized by serous detachment of the neurosensory layer at the macula. It has a relatively high recurrence rate and mainly affecting middle-aged males. The etiology and pathogenesis of the disease still remain ambiguous. But choroidal changes which increase choroidal vascular permeability are the basic pathology of CSCR. Different diagnostic methods such as FAF, FFA, OCT, OCTA, ICG could be used to detect its biomarkers such as choroidal thickness, choroidal vascularity index, hyperreflective dots for exact diagnosis and treatment response. Acute CSCR generally self-limited, but in recurrent or chronic forms may cause permanent visual loss due to progressive and irreversible damage in the photoreceptor layer of retinal pigment epithelium atrophy. Several treatment alternatives have been reported, such as PDT, intravitreal Anti-VEGF, TTT, Laser, Mineralocorticoid receptor antagonist for chronic and recurrent CSCR.
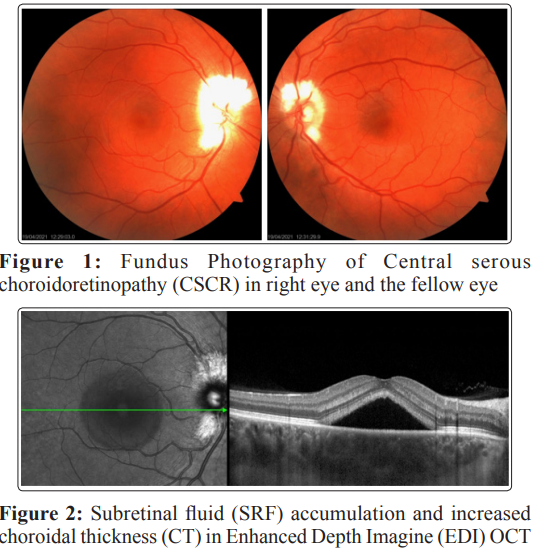
Central serous chorioretinopathy (CSCR) is one of the most common recurrent chorioretinal disorders characterized by the detachment of neurosensory retina with or without retinal pigment epithelial (RPE) detachment at the macula. Even its etiology and exact pathogenesis are not entirely understood. Choroidal changes play a major role, and CSCR is caused by leakage of fluid from the choroid due to increased choroidal vascular permeability (1-4).
Recently advanced Choroidal imaging techniques are essential for both the diagnosing and evaluation of treatment outcomes. Imaging biomarkers such as choroidal thickness, choroidal vascularity index, hyperreflective dots, which are quantifiable parameters, are fundamental for possible prognosis (1-5). Other several risk factors such as demographic and physiologic factors, lifestyle, and corticosteroid medication are the main predictive factors for the incidence of CSCR.
Even the acute stage of CSCR usually resolves spontaneously; the recurrent and the chronic forms have the risk of permanent vision loss because of retinal pigment epithelium (RPE) atrophy and irreversible photoreceptor destruction. Several different interventions have been published for chronic CSCR, such as several medications, subthreshold lasers, anti-vascular endothelial growth factor agent injection. Still, photodynamic therapy (PDT), seems to be the most effective method in these patients. (1-5)
The incidence of CSCR is higher in men than in women. Its incidence is changing in different populations such as reported that the incidence is 9.9 per 100,000 in men while it is 1.7 per 100,000 in women [5]. The male-to-female ratio was 6.5 in African Americans and 3.5 in Caucasian populations. Incidence and was found 9.75:1 in the Egyptian population. On the other hand, an epidemiologic study among the ages between 20 and 60 years in Taiwan demonstrated that CSCR was 1.7 times higher in men than in women [1,2,6,7]. The CSCR is predominantly seen in young and middle-aged individuals within their third to fourth decades with an average age between 39 and 51 years. Kitzmann and colleagues observed the incidence of CSCR was highest between the ages of 30 and 44 years in the USA [5].
Several risk factors such as psychological and physiological stress are related to the presence of CSCR; some of them are pregnancy, circadian rhythm disorders, corticosteroid medications, sleep disturbances, obstructive sleep apnea, irregular work schedules. CSCR is also correlated with personalities such as Type A personality, and narcissistic traits. Stress-induced psychological factors such as depression, somatization, hostility, alexithymia are related to CSCR [8-12]. The highest incidence rate was reported in 2011 from 2005 to 2012 time period which coincided with the economic crisis of 2011 in Greece [13].
Emotional stress caused caused by financial, social, and other psychological factors affected the development of CSCR. Similarly, irregular working hours were found to be as a potential risk factor for the development of CSCR. It is hypothesized that the choroidal vascular flow is dysregulated in patients with CSCR and during the either emotional or physical stress, the compensatory mechanisms of the autonomic nervous system are defective compared to normal eyes.
The relation between emotional stress and CSCR could be developed by stress-related increases in cortisol level. Endogenous corticosteroids, such as cortisol stimulates adrenergic receptors, leading to the release of endogenous epinephrine. Increased epinephrine release affecting the production of several mediators such as prostaglandins, free radicals and nitric oxide, resulting in increases choroidal blood flow and choroidal hyperpermeability. ICGA evaluation in eyes with CSCR showed the choroidal hyperpermeability that this finding supports the hypothesis about the correlation between emotional stress, corticosteroids, and choroidal hyperpermeability hypothesis [8-14].
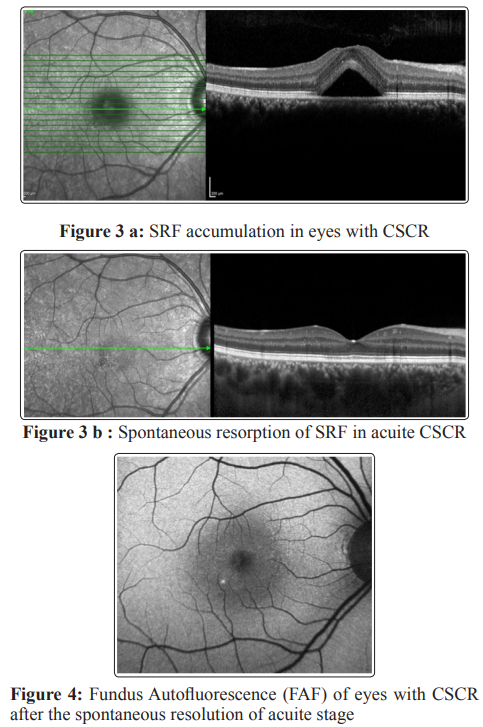
The Fundus Autofluorescence (FAF) photography is a noninvasive technique that shows the integrity of the retina by using stimulated emission of light from fluorophores such as lipofuscin. Phagocytosis of damaged photoreceptor outer segments by RPE causes the accumulation of lipofuscin. A normal healthy macula shows uniform autofluorescence without hyper and /or hypo autofluorescence area. RPE dysfunction causes the different patterns of FAF. A standard FAF pattern in CSCR has not been described yet, and it changes during the course of the disease [15-19].
The hypo autofluorescence in CSCR can be occure due to the alterations in RPE , that cause the subretinal fluid (SRF) accumulation. It is suggested that the hypoautofluorescence in CSCR correlated to areas of detached retina. On the other hand Hyperautofluorescence may be attributed to reduced phagocytosis of outer segments of photoreceptor by RPE that build-up of the potential lipofuscin precursors to produce autofluorescence [15- 19].
Evaluate the patterns of FAF changes during the course of CSCR. They reported that a gradual change in FAF patterns, from hypo autofluorescence to hyper autofluorescence. According to their evaluation, hypo autofluorescence could be due to SRF in the acute phase or reactivation. On the other hand, punctate hyper autofluorescence shows chronicity due to lipofuscin accumulation from outer segments of photoreceptors or macrophages which have phagocytosed ingested lipofuscin [18]. also described several FAF patterns in CSCR that the diffuse hyper autofluorescence which was the earliest Type that develops about four months after the first SRF accumulation, the most frequent one was the granular hypo autofluorescence, and other types were confluent hypo autofluorescence and punctate hyper autofluorescence.
Retina sensitivity (RS) that was evaluated by microperimetry was correlated with FAF findings such as hypo autofluorescence areas correspond to decreased RS while hyper autofluorescence areas may correlated either decreased or normal RS; on the other hand, absence of autofluorescence corresponds to absolute scotoma [19].
Fluorescein Angiography (FA) is one of the most valuable, dynamic imaging modalities for diagnosing CSCR. It shows retinal blood flow, leakage area, and leakage pattern. In the early phase of an FA, eyes with CSCR typically show either a single leakage point or multifocal leakage sides. The leakage sides are predominantly localized within or adjacent to the SRF area. The most common pattern ‘’ing point’’ leakage is ink-blot which is occure in 60% of eyes with CSCR. In comparison, the ‘’smoke- stack’’ pattern occurs in less than 30% of cases.
The angiogram shows early hyperfluorescence with progressively increase in both intensity and pooling. The ‘’smoke-stack CSCR pattern” was attributed to choroidal vasculature abnormality not the retinal pigment epithelium pathology. In contrast, multifocal leakage occurred due to diffuse retinal pigment epithelium abnormalities, and atrophy. Retinal pigment epithelium abnormalities are often seen as granular or mottled hyperfluorescence in mid-and late phase. The fluorescein leakage intensity was defined as the ratio between hyperfluorescent area at mid-phase to early stage, which is correlated with increased duration of a CSCR period. FA shows multifocal leakage with diffuse RPE abnormalities, and atrophy in eyes with chronic CSCR [1,7,20,21].
OCT is an essential non-invasive imaging tool in the diagnosis of CSCR. It can evaluate subretinal fluid accumulation, morphological alteration in neuronal layers, disturbance of external limiting membrane (ELM), morphological changes in the ellipsoid zone, and pigment epithelium detachment (PED), areas of both RPE atrophy and RPE hypertrophy which typically occur in chronic CSCR. OCT can be used to identify prognostic biomarkers like intra-retinal hyper-reflective dots, which usually progress from inner to outer retinal layers and correlate with poor visual prognosis. In addition, it can measure the central retinal thickness (CRT), choroidal thickness (CT), and choroidal vascularity index (CVI) [22-25].
The CT, which is measured from the posterior edge of RPE to the sclera-choroidal interface, is increased in eyes with CSCR and the normal fellow eye. Large choroidal vessels that are Sattler’s and Haller’s layers consist of up to 70% of overall CT. CSCR is characterized by thickened and enlarged large choroidal vessels, and they are compressed to choriocapillaris, the inner choroidal layers. A definitive cut-off point of CT to define CSCR as one of the pachychoroid spectrum disorders is not determined yet. Enhanced Depth Imagine (EDI) OCT significantly shows increased CT in the macula compared to the peripapillary region [22-25]. Found that the mean subfoveal CT was 450±66µm (range=356–595µm) in eyes with CSCR and 367±86µm (range=220–554µm) in the unaffected fellow eye.
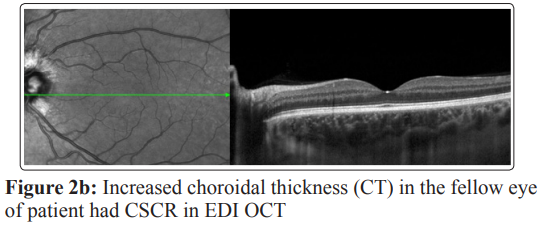
CVI, describe as the ratio of stromal area versus total choroidal area in either single-line or volume scans. CVI is increased in eyes with an acute state of CSCR compared to their fellow eyes as well as compared to eyes with resolved CSCR. In acute state of CSCR, engorgement of the choroidal vessel leading to an increased luminal area of the choroid that results in increased CVI. Therefore CVI can be accepted as a biomarker of disease activity. It was reported that the highest CVI was found in the nasal region, followed by the inferior, temporal, and superior quadrant. The least CVI was observed at the macula in healthy eyes [24]. Reported 88.9% of eyes had dilated outer choroidal vessels beneath the Ellipsoid Zone, and 66.7% of eyes had attenuation of choriocapillaris.
OCT demonstrated the quantitative changes such as cystoid macular edema (CME), cystoid macular degeneration (CMD), and flat, irregular pigment epithelium detachment, also known as the double-layer sign, all of which are not the unique signs to eyes with CSCR. Double-layer sign describes as the split between RPE and Bruch membrane that is predictive of type 1 macular neovascularization, which initially may be nonexudative. In OCT evaluation, eyes with CSCR show several types of PED, which may or may not be associated with SRF. The presence of SRF is not evidence of macular neovascularization. The flat, irregular PED; double layer sign in OCT is seen in chronic CSCR while serous PED is seen in acute or recurrent CSCR [1,22,23,25].
OCT examination revealed several other changes such as increased hyperreflective foci, presence of reflectivity irregularities, undulations, and thinning at the Ellipsoid zone /interdigitation zone (EZ/IE) zones adjacent to the sites of focal disruptions in CSCR. RPE atrophy was detected with the hyper transmission of signal in 81% of eyes with choronic CSCR (c CSCR) without SRF on OCT evaluation [24].
The OCTA is a beneficial non-invasive imaging technique that analyzes vascular structure in different blood vessel layers like the deep retinal layers or choriocapillaris. It also evaluates vessel density, microvascular alteration, choroidal vascular reactivity, and macular neovascularization in c CSCR. The prevalence of choroidal neovascularization in CSCR was estimated around 2%–9% before the development of OCTA. But in recent studies with OCTA showed 35% of eyes had a neovascular pattern [26- 28]. Reported that type 1 macular neovascularization was detected in 36.5% eyes with flat, irregular PED in CSCR with OCTA, compared to 25% eyes evaluated with combined FA/ICGA and spectral domain-OCT (SD-OCT). Furthermore, up to 25% of fellow eyes of chronic CSCR have a subtle macular neovascular membrane (MVM) which can not be detected on OCT evaluation.
ICGA is another valuable evaluation method in mapping the choroidal vascular structure for showing vascular abnormalities in CSCR, especially the chronic form. Early choroidal filling delay, large choroidal venous dilatation, and focal hypercyanosis due to focal leakage because of choroidal hyperpermeability are seen in ICGA. Photodynamic treatment (PDT) was applied to the area of leakage with the guide of ICGA that is the the hypercyanosens area identified at the mid-to-late phase of ICGA. In cCSCR affected area develops persistent hypercyanosis. CNVM can often develop in cCSCR seen in ICGA as new dilated choroidal vessels with associated hyperpermeability. The ICGA is a useful diagnostic tool for screening the treatment effect on both the leakage side and membrane secondary to CSCR [1,29,30].
CSCR usually has a good clinical prognosis with spontaneous resolution within the first three months. However, some patients may have persistent SRD or multiple recurrences and relapse episodes, resulting in a chronic form of the disease. Chronic CSCR can cause permanent visual loss due to persistent neurosensory retinal detachment, photoreceptor damage, and progressive RPE atrophy [31-33].
CSCR used to be classified as acute and chronic form. The acute form is the most common type, a self-limiting form that disappears in 3 months, while the chronic one lasts more than 4 or 6 months, even lasting more. But this classification seems too simplistic, which only relies on the duration of the SRF. Even though still no consensus has been available regarding the classification of CSC. The most accepted classification was suggested as follows:
The underlying pathophysiology of different clinical forms of CSCR is not completely understood yet; for this reason, to date, no consensus has been reached regarding its treatment methods. Several interventions are recommended as treatment options including, photodynamic therapy (PDT), intravitreal anti-vascular endothelial growth factor injection, subthreshold micropulse laser treatment, glucocorticoid antagonists, oral mineralocorticoid receptor antagonists. Due to its mostly self-limited character, observation is the most preferred approach in acute CSC. It has a relatively high recurrence rate. Therefore a close follow-up is necessary for timely treatment [30,32].
PDT is acted by releasing free radicals that damage endothelium and provoking long-term vascular remodeling, reduces choroidal thickness, and decreasing extravascular leakage by reducing the choroidal vascular hyperpermeability. The therapeutic effect of PDT is mainly exerted on dilated choroidal large vessels with leaving choriocapillaris unchanged. It has been reported that PDT parameters, initially used for neovascular age-related macular disease, caused several complications such as choriocapillaris hypoperfusion, choroidal infarction, and macular neovascular membrane (MNM) development [32-34].
Wu and colleagues postulated that the increased incidence of NMN could be due to ischemia-induced by full-dose PDT, which causes the release of VEGF [35]. They also observed that the development of choroidal neovascularization was correlated with larger than 2400µm PDT spot size, a post-PDT subfoveal CT of less than 310µm and the old age. According to the high risk of MNM development, the PDT parameters have been modified to enhance safety by either reducing the dose of verteporfin or fluency of laser application. Both modalities are safe and have similar efficacy in terms of SRF resolution, central macular thickness reduction, and BCVA improvement.
Arf and coworkers reported that SRF was resolved entirely in 100 % of eyes, and PED was resolved in 70 % of the eyes after the treatment with reduced fluence PDT [30, 36]. Observed that 80.0% of eyes showed complete resolution of subfoveal PED, 67.9% of subjects reported subjective visual improvement. In contrast, the mean visual acuity increased from 0.15 to 0.09 LogMAR 3 months after treatment with reduced-fluence PDT [37]. Found that Half-fluence PDT treatment is both safe and effective therapy in eyes with chronic CSC. They suggest that the most important predictive factor is baseline visual acuity [38]. Observed a significant decreased in Choroidal volume (CV) with PDT treatment that CV decreased from 9.35 ± 1.99 mm3 to 8.52 ± 1.92 mm3 at month 1 and 8.04 ± 1.7 mm3 at month three after the Half-fluence PDT post-PDT.
Anti-vascular Endothelial Growth Factor (anti-VEGF) Agents Even a significant increment of ocular VEGF levels in CSCR was not proved yet, and intravitreal anti-VEGF injections could have a potential therapeutic effect to reduce hyperpermeability and congestion of choroidal vessels. Several researches that analyze the anti-VEGF treatment’s effect, demonstrate significant reduction of CMT at 1, 6 and 12 months of follow-up compared to observation without any treatment. But anti-VEGF treatment does not show any significant effect on BCVA improvement. Intravitreal Anti- VEGFs have an effective therapeutic agent in treating MNM secondary to c CSCR [39-42].
Observed a similar efficacy of full-fluence PDT and IV anti- VEGF injections to treat cCSCR complicated with choroidal neovascularization [43]. Development of MNM was reported to be 4–8% of patients with chronic CSCR in most of the researches. But Wu and colleagues demonstrated the occurrence of choroidal neovascularization by OCTA in 45.7% of eye association with Ccscr [35]. Therefore intravitreal anti-VEGF treatment injection combined with the half-fluence PDT seems superior for treating CSCR complicated with MNM.
Laser photocoagulation treatment is used for sealing the RPE leakage sites. Suprathreshold laser treatment initially destructs the RPE at the leakage site that stimulates proliferation and ingrowth of the surrounding healthy RPE and facilitates the SRF resorption. Laser photocoagulation is also effective for improvement in vision. However, it is not suitable for CSCR with subfoveal leakage site because of laser-induced scar and successive central scotoma. Suprathreshold laser treatment does not decrease the recurrence rate and not predictable results compared to other treatments like PDT or anti-VEGF.
On the other hand, Subthreshold micropulse laser (SML) demolish only RPE cells, by producing a high peak temperature in intracellular melanosomes of RPE that cause cellular membrane rupture of only RPE cells. The 577 nm SML only minimally absorbs by xanthophyll pigments located in the macula’s inner and outer plexiform layers. This way, SML can generate the same biological effect of suprathreshold laser treatment without destruction in photoreceptors. Therefore SML treatments near the fovea are relatively safe comparing to suprathreshold laser treatment in terms of lack of development of subfoveal scar and central scotoma [32,44-47].
Reviewed 12 research about SML treatment in CSCR persisting for more than four months and reported that 79.6% of eyes had reduced CMT, and 63.6% showed a complete resolution of SRF [45]. On the other hand, CMT reduction was observed in 39%, and a complete resorption of SRF was detected only in 8% of the untreated control group [46]. In review, the mean CMT reduction was 80μm, and a BCVA increment was nine letters with a median follow-up of 12 months. reported that CMT decreased from 369 to 250 μm with 577 nm SML with a median follow-up time of 18 months [47].
PLACE trial results showed that the SRF resolution rate was 51.2% with half-dose PDT treatment while only 13.8% in SML treatment at the first post-treatment examination at 6–8 weeks. Furthermore, eight months after the treatment, SRF resorption was observed in 67.2% of eyes in the PDT group vs 28.8% in the SML treatment group [48]. In the PLACE trial, the improvement in vision-related quality of life seems similar for both half-dose PDT and SML treatments. Therefore both treatments choose to appear to be effective treatments alternatives for chronic CSCR [48].
MR receptor activation in the sensory retina causes smooth muscle cells relaxation in the choroidal vasculature, choroidal vasodilation, and leakage due to upregulation of the calcium- dependent vasodilator potassium channel. Similar ophthalmologic symptoms have been observed in the patient with primary hyperaldosteronism [32]. MR antagonists, either spironolactone or eplerenone, could be a potential effect on CSCR treatment. It is recommended to administer 25 mg oral eplerenone for a week as an initial dose, followed by a 50 mg dose daily, if no adverse effects such as hyperkalemia, myotonia, bowel irritation have occurred. However, the clinical results are controversial [49].
Reported that even the BCVAs were improved with MR antagonist treatment for 12 months, CMT decrement and SRF resorption were not significant. Observed a complete SRF resolution in 29% of eyes, a transient SRF reduction in 33% of eyes after a median of 106 days. In their study, 25% of eyes did not have any response [50]. Furthermore, 13% of patients had the significant adverse effect of MR antagonists.
Diode laser with the wavelength of 810 nm mainly absorbs by the choroid. Therefore Transpupillary Thermal Therapy (TTT) could have a promising useful, and cost-effective therapeutic choice in chronic CSCR. Further investigations with TTT are needed to find out treatment parameters for both long-term efficacy and safety [32]. Anti-androgenic drugs, Methotrexate (MTX), Rifampicin, and Melatonin, are other alternative treatments for chronic CSCR, but further studies with a large number of patients and more extended studies are needed to prove their use in clinical practice [32].
CSCR is one of the most common retinal disorders, but its exact pathophysiology is not entirely explained yet. Several biomarkers of CSCR can be evaluated by the recently developed advanced multimodal imaging techniques such as OCT, EDI OCT, OCTA, ICGA. With the help of these technologies in addition to early and correct diagnosis, treatment outcomes can also be evaluated
