Author(s): Chhavi Mehra*, Annie Mattilda Raymond and Sunil L
Background: Type 2 diabetes mellitus (T2DM) is not only one of the leading causes of mortality, but its impact on healthcare costs and burden is
becoming unsustainable each year. The quality of life and life expectancy are both significantly impacted by this chronic metabolic condition. To help control their blood glucose levels, patients with T2DM adhere to a self-management regimen as instructed by a professional. Various technological options are available now to help self-management.
Methods: Here, we present a case of a 64-year-old female with insulin-dependent type 2 diabetes mellitus, multiple co-morbidities, depression, confined to her room, and inability to walk for about a year. After six months of the Sugar fit approach with daily-personalized life coaching, expert medical advice, tech-enabled, AI-driven model, she showed tremendous improvement in every parameter.
Results: Before joining sugar fit, the patient was on 44 units of rapid insulin and 18 units of long-acting and oral anti-diabetic medications. The patient’s Hba1c at baseline was 8%; six months later, it is 6.8% with all rapid and long insulin stopped and oral meds essentially the same as before. She has reduced creatinine from 1.88 to 1.37 and triglycerides from 1015 to 448, respectively. Her BP medications have been reduced to 50%. She walks for 2 km every day and is socially active with resolved depression. She has lost 3 kgs of weight and 3 inches of waist circumference.
Conclusions: The findings indicate that a tech-enabled, AI-driven model with intensive, personalized coaching, lifestyle modification, and expert
physician guidance has shown remarkable results even in this particularly complicated case.The findings indicate that the personalized and individualized frequent lifestyle coaching and expert physician opinion enabled by superior technology and AI-driven Insights resulted in marked improvement of all parameters and significant medication reductions even in Diabetes of long duration
with comorbidities.
A significant concern globally is type 2 diabetes mellitus (T2DM), defined by the disruption of glucose homeostasis [1, 2]. Type 2 diabetes mellitus (T2DM) is a metabolic syndrome with a bundle of chronic degenerative diseases. Diabetes that is not managed well results in vital organ complications, contributing to a high mortality rate. Four hundred twenty-five million people were affected by diabetes in 2017. By 2030, this number is expected to rise to 578 million, from 463 million in 2019 [3, 4]. Increasing age, rising BMI, a sedentary lifestyle, a lack of physical exercise, poor diet, and stress are all known risk factors for T2DM [5]. Chronic hyperglycemia poses a significant health risk and economic burden for the person and society because it can harm multiple organ systems [6, 7]. The burden of the disease is determined by the prevalence, lifetime risk, and concurrent co-morbidities. Microvascular and macrovascular consequences, such as coronary heart disease, myocardial infarction, stroke, retinopathy, neuropathy, nephropathy, and arterial occlusive disease, are particularly significant. With sharply rising healthcare expenditures, these consequences directly affect the patient and society at large [8]. Since there is a substantial correlation between getting older and T2DM, approximately half of all persons with diabetes are now older adults [9]. In contrast to younger adults, older adults exhibit more considerable diversity of physical and cognitive ability. Comorbidities, an increased propensity for hypoglycemic episodes, specific care requirements, and a loss of resilience that might increase the likelihood of frailty further add to the complexity of sickness treatment in older people [10]. Worldwide, there is a sharp rise in the proportion of older adults who have T2DM; this development is primarily attributed to longer life expectancy following long-term prior exposure to cardiometabolic risk factors, particularly excess body fat, skeletal muscle atrophy, and decreased levels of physical activity [11-13].
T2DM can cause functional impairments in daily life and a severalyear reduction in life expectancy. It is a disease where the control of sugar levels in the body is disturbed due to the pancreas's under-functioning or underproduction of insulin. It has many sub classifications, out of which Type 1 and Type 2 DM is the most prevalent; type 2 DM can somehow be managed with a healthy lifestyle. When there is no effective treatment for diabetes, the best course of action is to focus on maintaining healthy, normal blood sugar levels by adhering to a balanced diet, frequently exercising, taking medicine as directed, and getting regular examinations with a doctor. Since diabetes is a chronic condition with no known cure, self-management becomes essential to managing the disease. An effective self-management program can help people control their diabetes and prevent unnecessary problems arising from poorly managed or uncontrolled diabetes. An excellent regimen tailored to each patient's needs sometimes even works to permanently reverse type II diabetes [14]. Patients with diabetes who want to self-manage their condition should generally monitor their blood sugar levels and blood pressure daily and keep them within the target ranges, eat a healthy diet that emphasizes foods with a low glycemic index (GI), exercise regularly, reduce their weight if it is above the recommended range, and give up smoking. Although self-management programs can help manage diabetes, a survey of more than 100 diabetic patients revealed that a technologically based solution might help people manage their condition more effectively [15].
Here is a case study presenting remarkable improvements in all parameters in a long-term T2DM patient with multiple chronic comorbidities by Sugar fit’s -Tech/AI-driven platform with daily-personalized life coaching and expert medical advice. The platform intends to encourage patient self-management and give them the tools to make long-lasting behavioral changes. To our knowledge, this study is the first used Tech/AI-driven intervention in T2DM management concerning medical advice and personal life coaching.
The objectives of the study were to identify the critical issues of the user to deliver appropriate, personalized, and effective clinical treatment along with empathetic coaching, Prove the efficacy of an end-to-end program for a sustainable reversal that leads to beta cell recuperation, metabolic recovery and reduction of endorgan complications from diabetes and to share experience and knowledge with peers.
Biography - A 64-year-old female with a history of diabetes for 20 years and multiple complications like hypertension, dyslipidemia, grade 3 fatty liver, hyperuricemia, and osteoarthritis. The patient was overweight and had mood disorders, a history of ischemic heart disease, and non-alcoholic steatohepatitis. The patient also suffered from severe anxiety, tiredness, and possibly clinical depression.
Sugar Fit’s Interventions: Management of T2DM with AI-driven Sugar fit approach, along with daily-personalized lifestyle management and expert medical advice. In 9 months, six doctor consultations and six coaching sessions were done over video calls, 87 audio consultations with the coach, 800+ texts exchanged between coach and client, and about 223 SMBG (Self-monitoring of blood glucose) readings were recorded over the Sugar fit app.
It lasted three weeks and was a multiple-step process with basic and advanced assessments. For starters, blood and urine tests, weight measurement, glucometer readings, smartwatch integration, and vitals check. A continuous glucose-monitoring device and smart goal tracking followed this. The data of metabolic markers were also collected. Most importantly, a regular check of the patient’s compliance with dietary modifications was done. The outputs of this phase include precision nutrition, progressive exercise, improved sleep quality, and a beginning of mindfulness in the patient’s attitude. The patient was guided with what, when, and how much to eat. Gradual progression from an inactive lifestyle was done to break the movement inertia through interventionbased progress. Through routine, sympathetic counseling for long-lasting habits, they could eliminate the patient's cravings. This will lead to recovery of beta-cell function in the long term; accumulation of glucose and overflow of blood vessels and cells can be prevented, which leads to reduced inflammation, and insulin action will be optimized through the recovery of receptor structure. Along with this, excess fat generation in the liver can be prevented, and the gut microbiota community improves.
The control over glycemic levels was targeted with precision nutritional counseling and progressive fitness routines. The patient did rigorous SMBG checks, and health coaches gave insights on regular phone calls on personalized lifestyle interventions.
Diet - Nutritional interventions include a few easy tweaks and modifications so that it can be a sustainable change. Like having a medium bowl of salad before lunch and dinner, swapping juice with whole fruits, sticking to meal timings, including millets on alternate days, increasing vegetable intake, including a glass of buttermilk every day, and swapping processed snacks with fruits.
stro Physical Activity - Fitness interventions are equally important to see visible changes. They started with slow walking for 5 minutes after meals and gradually increased the time to 10 and 15 minutes, including chair yoga routines and ‘starters belly workout’ routine from the Sugar fit app. Exercises like stationary bicycling and leg raises were also incorporated into the practice.
Mindfulness - To implement a healthy lifestyle, it is also crucial to make some mindfulness interventions. Eating dinner an hour early and sleeping on time. There should be at least 10 hours of gap between dinner and breakfast, gradually increasing the gap to 12 hours. Practice yoga-nidra routines from Sugar fit app to improve the quality of sleep. Check fasting glucose levels on a glucometer daily and record them on the app.
The patient's energy levels were low at the program’s start, but they have improved tremendously over six months, and the tiredness has reduced. Sleep quality and consistency are also enhanced. The patient could not walk and hardly moved, but now she can walk 3000 steps with ease and 15 minutes of stationary bicycling and half an hour of yoga daily.
Social behavior has improved over time. She used to be moody, stayed locked in a room, and had no interest in meeting family or friends. Now, she is happier, meets people, and even goes grocery shopping (Table 1). Regular follow-ups and regular selfmonitoring of blood glucose have been very effective.
| Parameters | Baseline | After six months in Sugarfit |
|---|---|---|
| Energy | Low | Improved |
| Sleep | Disturbed | Improved |
| Tiredness | Severe | Nil |
| Fitness | Inability to walk, hardly moved | Could walk 3000 steps with ease along with 15 minutes of stationary bicycling and half an hour of yoga every day |
| Social behavior | Moody, locked in the room, no interest in meeting friends/ family | Happy, socialize people and goes grocery shopping!!! |
| Diabetes management | SMBG nil, no frequent follow-ups | Daily 1 SMBG, frequent follow-ups |
In this study, a 64-year-old female patient diagnosed with T2DM was enrolled and adhered to nine months of personal coaching, guidance from a diabetes expert health and fitness coach, and a doctor. The patient was monitored for fasting blood sugar, haemoglobinA1c (HbA1c) level, triglycerides, total cholesterol, HDL, LDL, creatine, and uric acid.
Overall, there is a tremendous improvement in the patient’s blood profile and a considerable medication reduction. The patient had an HbA1c level at a baseline of 8. After nine months into the intervention, HbA1c dropped to 7.4 at three months, 6.8 after six months, and finally, it reduced to 6.7 after nine months. The patient’s fasting blood sugar was 184 at baseline. After nine months of intervention, the fasting blood sugar was reduced to 107. Insulin has completely stopped in 9 months, and the medications have declined over nine months (Figure 1). Personalized interventions concerning behavioral modifications, physical activities, and diet significantly impact weight management and HbA1c levels [16]. The results revealed that the individualized intervention with a tech-driven approach significantly improved the HbA1c and fasting blood glucose levels.
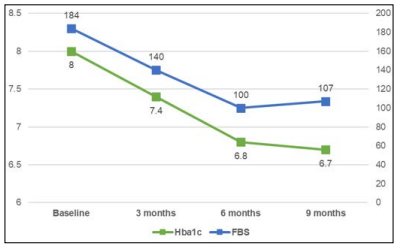
Figure 1: Change in mean fasting blood sugar and hemoglobin levels in the study
The lipid profile revealed that the total cholesterol has remarkably reduced from 251 to 189 after nine months, and triglycerides from 1075 to 812 in 6 months. However, it was reduced to 203 mg/dl in 3 months; it went up, possibly due to reduced dietary adherence, LDL has come down to 83 from 123, and HDL improved to 25 from 27. (Figure 2)
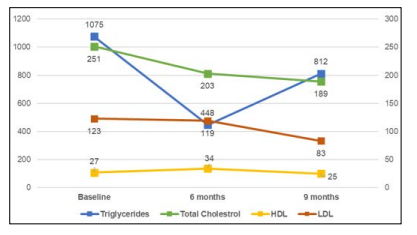
Figure 2: Lipid profile of the patient’s before and after the study
The creatinine levels of the patient have reduced from 1.88 to 1.31, and uric acid has dropped down to 3.5 from 7.9 (Figure 3)
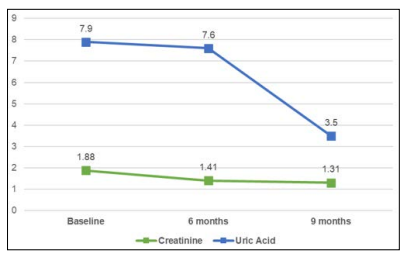
Figure 3: Creatinine and uric acid levels of the patient’s before and after the study
The body weight changes from baseline after a nine-month study. The baseline weight was 62, reduced to 59 kgs, and the patient lost 3% or more of her initial body weight. An inch loss has been noticeable, with the waist dropping 5 inches (Table 2). The average BP at baseline was 175/100, and it was reduced to an average BP of 135/85 at three months and has been in a similar range since.
| Parameters | Baseline | 3 months | 6 months | 9 months |
|---|---|---|---|---|
| Weight | 62 | 61 | 60 | 60 |
| Waist | 104 | 101.6 | 101.6 | 99.06 |
| BMI | 25.8 | 25.4 | 24.9 | 24.9 |
| Waist to height ratio | 0.67 | 0.65 | 0.65 | 0.65 |
Glycemic medications saw tremendous improvement. Long-acting insulin (Tresiba) was reduced from 18 units to 6 units in the first 90 days, remained at 6 units for the next 180 days, and was discontinued at the beginning of the 9th month (270 days from the starting of the Sugarfit’s personalised diabetes reversal program). While long-acting insulin took time to be eliminated from the patient’s medication routine, short-acting insulin (Actrapid) was eliminated in the first three months. Oral hypoglycemic agents like Janumet 50/500, which is a combination of Gliptins and Metformin remained the same until six months. They were changed to Ondero Met 2.5/500, which is a combination of Linagliptin and Metformin (Table 3).
| Meds | Baseline | 3 months | 6 months | 9 months |
|---|---|---|---|---|
| InsulinTresiba | 0-0-18 | 0-0-6 | 0-0-6 | 0 |
| InsulinActrapid | 16-12-14 | 0 | 0 | 0 |
| Janumet50/500 | 1-0-1 | Same | Same | Onderomet 2.5/5001-0-1 |
| Jardiance25 | 1-0-0 | Same | Same | Same |
Medications for lipids and NAFL saw good improvement as well. ‘Fenofibrate’ 145 mg and ‘Lasix’ 40 were stopped at three months. ‘Evion’ 600 was started at the beginning of 3 months and reduced to 400 at the beginning of 9 months. ‘Clopitorva’ 20 and ‘Flavedon MR’ remained the same from the beginning. ‘Lipaglyn’ 4 was started at the beginning of 3 months and increased to 8 mg at the beginning of 9 months. As per the cardiologist’s recommendation, ‘Prolomet XL’ 50 BD was changed to ‘Nebicard LN’ 5 once a day, and ‘CilacarT’ one tablet a day was changed to ‘Telma D’ one tablet a day (Table 4).
| Meds | Baseline | 3 months | 6 months | 9 months |
|---|---|---|---|---|
| Fenofibrate 145 mg | 0-0-1 | stopped | - | - |
| Lipaglyn 4 | - | 0-1-0 | Same | Increased to 8 mg |
| Evion 600 | - | 0-0-1 | Same | Reduced to 400 |
| Clopitorva 20 | 0-0-1 | Same | Same | Same |
| ProlometXL 50 | 1-0-1 | same | Changed as per cardiologist | Nebicard LN 5 1-0-0 |
| CilacarT | 1-0-0 | same | Changed as percardiologist | Telma D1-0-0 |
| Lasix 40 | 1-0-0 | Same | Stopped | Stopped |
| FlavedonMR | 1-0-1 | Same | Same | Same |
The Fibroscan done at baseline showed a grade 3 fatty liver. A
repeat Fibro scan at six months from the same Radiologist was
grade 2.
We saw the glycemic variations were more in time in range than
before, and hypoglycemic episodes had resolved entirely
The stellar tech-driven approach is a technology-enabled coachled doctor-monitor program. During the entire nine months of the study, the health coaches collected data at set intervals about the patient’s food intake, physical activities, height, weight, sleep quality, and waist circumferences. The health coaches also monitored and communicated to the expert physicians on the platform about the patient’s blood sugar level, HbA1c, total cholesterol, HDL, LDL, triglycerides, creatinine, and uric acid levels.
Lifestyle diseases like obesity, cardiovascular disorders, diabetes, and hypertension are at an all-time high and growing significantly. Poor metabolic health is the root cause of most conditions; continuous motivation, habit formation, and personalization are essential. Originally, adipose tissue was classified as a simple energy storage organ, but it is known to function as a primary endocrine system that secretes adipokines, growth factors, cytokines, and chemokines. When the capacity of adipose tissue is overwhelmed, fat accumulates in ectopic sites such as visceral depots, liver, skeletal muscle, and pancreatic beta cells. This leads to inflammation, followed by insulin resistance and finally metabolic syndrome. Visceral adiposity is strongly associated with insulin resistance, diabetes, dyslipidemia, hypertension, and non-alcoholic fatty liver disease.
Recent epidemiological evidence shows that 85% of type 2 diabetic adults are obese or overweight. In obesity, adipose tissue becomes dysfunctional, promoting a pro-inflammatory, hyperlipidemia, and insulin-resistant environment contributing to type 2 diabetes mellitus (T2DM). Concurrently, similar features that result from adipose tissue dysfunction also promote cardiovascular disease (CVD) by mechanisms that T2DM can augment. The mechanisms by which dysfunctional adipose tissue simultaneously promotes T2DM and CVD are adipose tissue depot-specific adipokines, inflammatory profiles, and metabolic dysfunction.
The loss of visceral fat is associated with reduced fasting glucose and insulin levels and CVD risk factors, including reduced systemic inflammation, total cholesterol, LDL cholesterol, and triglycerides. Studies have shown that modest weight loss due to dietary changes in people with overweight or obesity is due to roughly equivalent fat loss from subcutaneous and visceral depots. At the same time, the addition of exercise leads to more weight loss from ectopic fat accumulation.
It is well established that aerobic exercise increases fuel mobilization from adipose tissue by increasing lipolysis and subsequent FFA (free fatty acid) mobilization, ultimately decreasing adiposity and adipocyte size. Such enhanced fuel mobilization is thought to be highest for visceral WAT. Several studies have shown that a high level of fitness (defined by a high activity level with maximal oxygen uptake) is negatively associated with visceral adiposity. It has been suggested that prolonged sustained weight loss can lead to improvements in adipose tissue inflammation that were not observed in the same subjects following acute moderate weight loss. Weight loss achieved through calorie restriction and exercise resulted in decreased systemic IL-6, CRP, TNFα, MCP-1, soluble intercellular adhesion molecule-1 (ICAM-1), and vascular cell adhesion molecule-1 (VCAM-1)
AI-driven models with intensive, personalized coaching, lifestyle modification, and expert physician guidance have shown remarkable results even in this particularly complicated case. We studied for the first time that T2DM could be reversed using AI-driven model intervention, including health coaching, medical management by expert physician guidance and emphasizing nutrition education without going extreme/FAD routes.
The authors gratefully acknowledge the operations team, product design, and engineering team for offering a hassle-free and best patient experience. We especially thank Coach Nikita Mendonza for helping in data collection, analysis, and care delivery.
This study was funded by Ragus Healthcare Private Limited (sugarfit), Bengaluru, India.
Client data taken for this study was duly informed about publishing this data for study purposes. The client consented to participate in the program.
