Author(s): <p>Dhatri Kallala*, Balaji Varaprasad Mallula, Srinadh Boppana, Santhosh Jitta and Govardhan Das Joel</p>
Radiological imaging plays a crucial role in the diagnosis and management of a wide range of abdominal pathologies, including those affecting the omentum and mesentery. The omentum and mesentery are important structures in the abdominal cavity, serving a variety of functions, such as providing support to the gastrointestinal tract and facilitating the flow of lymph and blood. Pathologies affecting the omentum and mesentery can result in a wide range of clinical presentations, from mild discomfort to life-threatening complications. Omentum and mesentery are involved in various benign and malignant pathologies like omental infarction, omental torsion, encapsulated fat necrosis, fat saponification due to trauma or pancreatitis, mesenteric panniculitis, epiploic appendagitis, omental nodules and caking in infective and malignant conditions like tuberculosis, peritoneal carcinomatosis and metastasis. Sometimes, there exists a diagnostic dilemma between the benign condition like focal encapsulated fat necrosis and malignant condition like liposarcoma, localized peritoneal carcinomatosis. Therefore, Radiological imaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI), are invaluable tools for the diagnosis of omental and mesenteric pathologies. In this context, radiologists play a vital role in the accurate interpretation of imaging studies, enabling timely and appropriate management of these complex and often challenging conditions.
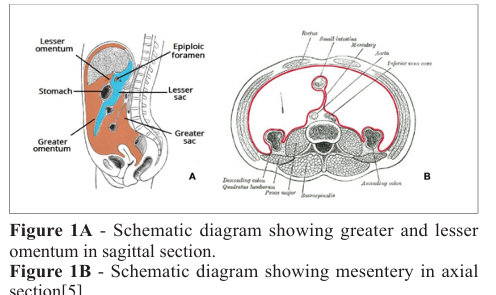
Peritoneum is the largest serous membrane of the human body, formed by parietal peritoneum that lines the abdominal cavity and visceral peritoneum, that envelopes abdominal viscera [1, 2]. Peritoneal reflections like omentum, mesentery and intraabdominal ligaments interconnect the viscera with in the abdominal cavity.
Omentum is a predominantly fat-containing sheet containing nerves, blood vessels, lymph channels, connective tissue and fat, present between stomach and other organs. There is greater and lesser omentum. Greater omentum aka epiploon is formed by double layer of peritoneum (4 layers in total) that hangs down from greater curvature of stomach and 1st part of duodenum for a variable length and folds back to finally insert on the anterosuperior surface of transverse colon [3]. Similarly lesser omentum extends from the lesser curvature of stomach to the ligamentum venosum in the liver.
Mesentery is a double layered peritoneal tissue that connects small bowel, portions of the colon to the posterior abdominal wall. It contains adipose tissue, superior and inferior vessels and branches, lymphatics [4]. Small bowel mesentery, transverse and sigmoid mesocolon correspond to the name of the organ it connects to the posterior abdominal wall.
Peritoneal reflection pathologies are mostly overlooked as they are missed during the 1st line of investigation, ultrasound and have gained interest due to the increased role of computed tomography in the diagnostic imaging.
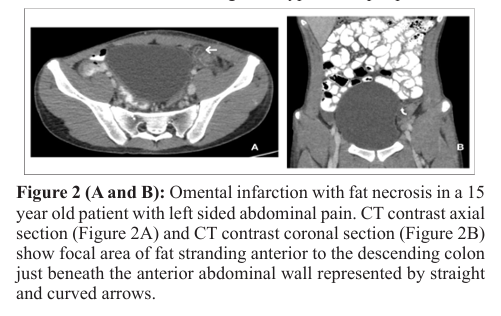
Omental infarction with or without torsion is a well-recognised cause of acute abdominal pain which is rarely diagnosed on ultrasound. It is commonly seen in the right lower abdomen, adjacent to the caecum, inferior to the liver due to higher mobility and greater length on the right side. Omental infarction results due to a kink in the venous channel or by omental torsion itself [6]. The cause of primary omental infarction is usually idiopathic whereas secondary omental infarction is seen post surgery, trauma or inflammation. Patients present with abdominal pain which is not associated with gastrointestinal symptoms or fever [7]. Sudden abdominal pain in runners, marathoners and healthy individuals should raise the suspicion of omental infarction due to low omental blood flow. It is usually self limiting and treated with analgesics conservatively. Auto amputation is one of theconsequences during resolution due to fibrosis and retraction. When encountered, complications like abscess formation necessitate surgical intervention. USG may not be very helpful in diagnosing omental infarction. If seen it is visualized as a focal area of hyperechogenecity in the omentum. CT scan is the imaging modality of choice for omental infarction, which is seen as a focal area of fat stranding with hyperdense peripheral halo.
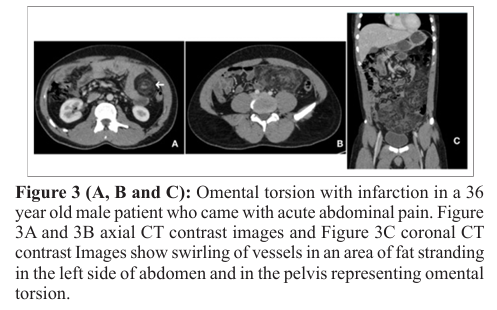
Omental torsion is one of the rare causes of acute abdominal pain. Twisting of the omentum along the long axis, compromising the vascular supply, results in omental torsion [8]. Primary omental torsion is seen in the absence of any intra-abdominal pathology and the thickened segment of omentum rotates around the proximal fixed point. Etiology of primary omental torsion is not well known and is assumed to be due to omental anomalies like bifid omentum, accessory omentum, anomalous vascular supply and kinking [9]. Secondary omental torsion is seen in patients with pre-existing intra-abdominal pathologies like inguinal hernia, abdominal wall hernias, tumors or cysts, post-surgical wound. Factors increasing the intra-abdominal pressure like coughing, labour, lifting heavy weights, heavy meals, forceful vomiting displace the omentum and predispose to omental torsion [10]. Acute appendicitis is the major clinical differential diagnosis of omental torsion.
If visualized on ultrasound, omental torsion is seen as a complex mass with hyper and hypoechoic areas with or without intraperitoneal free fluid. CT abdomen has high sensitivity for omental torsion and seen as omental haziness with whirling of omentum in concentric pattern around central blood vessel (whirl sign). Recurrent episodes of incomplete omental torsion result in omental ball formation, thickened fibrosed omentum. In most cases, it is self limiting, unless it is huge or secondary to an underlying pathology.

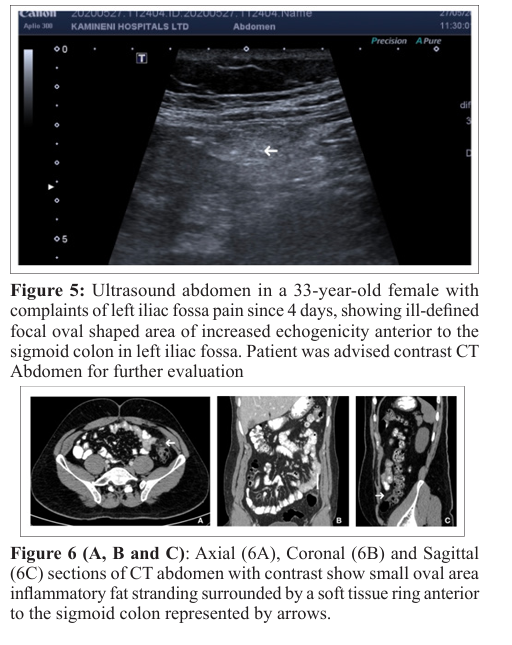
Epiploic appendages are benign peritoneal outpouches that arise from the serosal surface of the colon which contain adipose tissue and vessels. Epiploic appendagitis is more commonly seen in the left colon and cecum and can measure upto 5 centimeters in length. The rectum does not contain any epiploic appendages. Inflammation of epiploic appendages is a resultant of torsion of epiploic appendages with vascular occlusion. Patients usually present with acute left sided abdominal pain. On ultrasound it is visualized as a round, noncompressible hyperechoic mass without internal vascularity, surrounded by a subtle hypoechoic line. On Computed tomography it is visualized as a fatty central core abutting the colon wall with surrounding inflammatory changes and a thin hyperdense rim-Hyperattenuating rim sign [11]. Presence or absence of central dot of high attenuation representing thrombosed vessels [12].
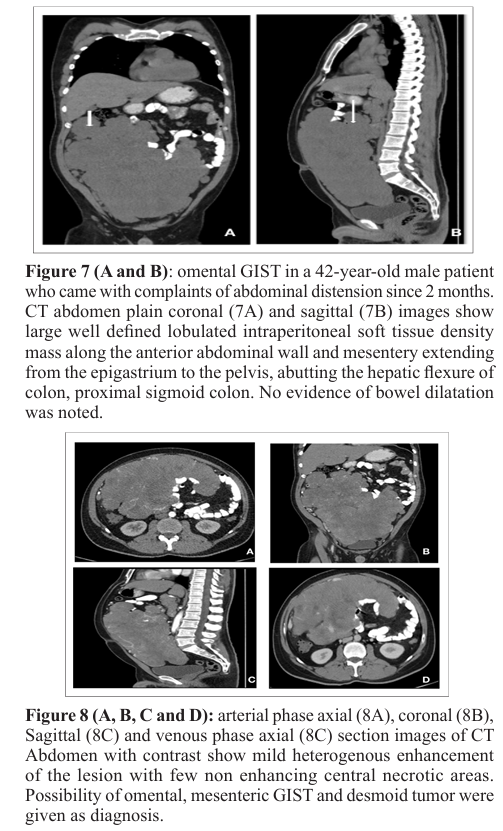
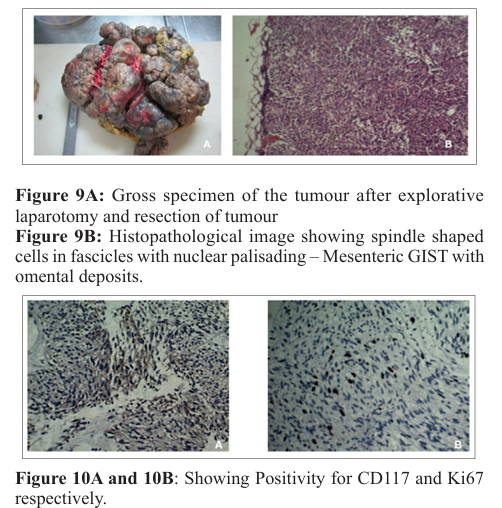
Gastrointestinal stromal tumours are benign/ malignant mesenchymal tumours of Gastrointestinal tract, most commonly arising from stomach and small intestine [13]. Extra gastrointestinal stromal tumours can arise from mesentery, retroperitoneum, omentum, liver [14]. Omental GIST is not a common entity. Patients usually present with complaints of abdominal pain, distension, fatigue, making the early diagnosis difficult and are diagnosed at larger sizes. Majority cases of omental GIST arise from the greater omentum are large sized (usually >10 cm). Prognosis of extra gastrointestinal stromal tumors is worse compared to gastrointestinal stromal tumors. These are KIT + and KIT/PDGFRA mutation driven mesenchymal neoplasms [15]. On plain radiograph it can be seen as soft tissue opacity displacing the bowel loops in case of large tumors. On ultrasound It is seen as large tumor with heteroechogenecity and central necrosis but it is difficult to identify the organ of origin. Computed tomography is used for definite diagnosis, and visualized as soft tissue density mass with central areas of necrosis, seen as fluid fluid level. Calcifications are uncommon. On contrast administration, mild enhancement of the peripheral non necrotic component is seen. Treatment is usually by En block resection and chemotherapy with Imatinib.
Normal omentum has attenuation similar to fat, therefore any disease process in the omentum makes it evident. When the omentum is affected by an inflammatory/ infectious/ neoplastic disease process, the initial response is by omental thickening, nodules which later progresses to form a mass which is referred to as omental cake [16]. Common malignancies associated with omental caking are ovarian malignancy, pseudomyxoma peritonei, stomach and small bowel carcinomas [17].
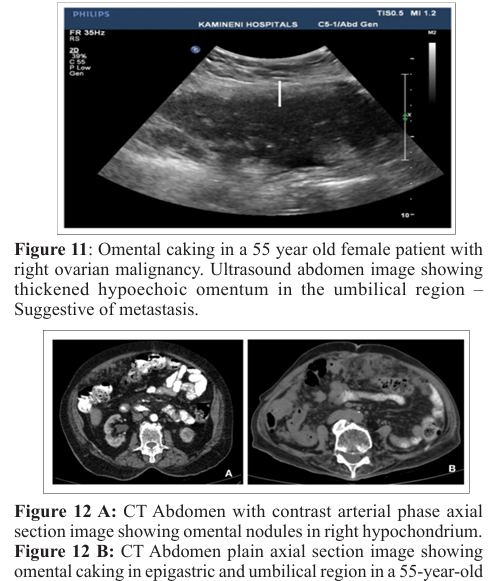
female patient with known history of right ovarian carcinoma.
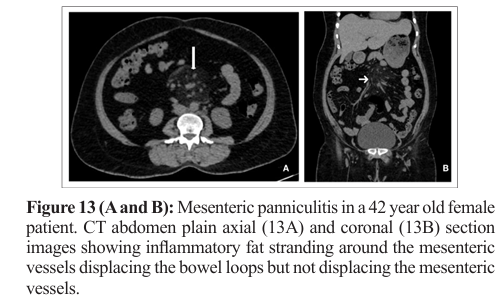
Mesenteric panniculitis is a benign and chronic inflammatory condition of unknown origin, involving the small intestine or colonic mesentry [18]. It is classified according to pathological changes (i) Chronic nonspecific inflammation, (ii) fat necrosis and (iii) fibrosis. If inflammation and fat necrosis are predominant, the condition is known as mesentric panniculitis. When fibrosis and retraction are predominant it is known as retractile mesentritis [19]. On computed tomography the imaging features are high attenuating mesentric fat, mass effect on neighbouring bowel loops, presence of lymph nodes, hypoattenuating halo sign surrounding the vessels and lymph nodes, hyperattenuating pseudocapsule [20].
Intra-peritoneal encapsulated fat necrosis (IPEN) is a rare condition in which Post traumatic or ischaemic insult results in fat degeneration encapsulated within a fibrous capsule in the peritoneal cavity. On CT scans, IPEN typically appears as well-circumscribed, round or oval-shaped mass that is iso-or hypodense relative to adjacent fat tissue. It can be located anywhere within the peritoneal cavity, but is most commonly found in the omentum or mesentery. The fibrous capsule around the necrotic fat is seen as a thin or thick rim of soft tissue density. In some cases, calcifications may be present within the capsule. On ultrasound, IPEN is seen as a heterogeneous, hypoechoic mass with internal echogenic foci and hyperechoic fibrous capsule, with occasional acoustic shadowing. Mild mass effect on the adjacent organs and enhancement of the fibrous capsule in encapsulated fat necrosis on contrast enhanced computed tomography mimics liposarcoma or peritoneal carcinomatosis [21]. Clinical history of the patient is critical in differentiating it from liposarcoma, as patients with encapsulated fat necrosis have a history of surgery/ trauma. Temporal evolution also helps in differentiating the two entities, as encapsulated fat necrosis decreases in size over time. IPEN is typically a benign condition that does not require treatment unless it is causing symptoms or complications such as bowel obstruction.
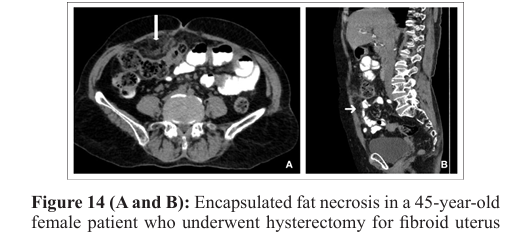
15 days back. CT abdomen plain axial (14A) and Sagittal (14B) images show well defined encapsulated area of fat necrosis in the right Para median location in the infraumbilical region.
A number of mechanical, inflammatory, infective and neoplastic pathologies affect the omentum and mesentery. A thorough understanding of radiological appearance of these conditions is crucial for accurate diagnosis and effective treatment of various abdominal conditions. In case of fat necrosis mimicking liposarcoma and peritoneal carcinomatosis, prior imaging and clinical history helps in the correct diagnosis of fat necrosis.
