Author(s): Mohammad Ali Alshami
ABSTRACT: Blue rubber bleb nevus syndrome is a rare, sporadic, congenital disorder characterized by numerous cutaneous and internal venous malformations. We report the case of a 2-month-old male with multiple large, bluish, bleb-like, nodular lesions on the face, scalp, neck, trunk, and limbs present since birth. Some of these lesions exhibit central ulceration, which is an unprecedented observation.
Blue rubber bleb nevus syndrome (BRBNS), also known as Bean syndrome, is a rare, sporadic, congenital, cutaneo-visceral disorder, primarily characterized by cutaneous and gastrointestinal tract (GIT) venous malformations (VMs), although any organ can be affected by this [1]. BRBNS may manifest at birth (30%), in infancy (9%), or during early childhood (48%), and may even be present prenatally [2]. Because only approximately 350 cases have been reported worldwide, BRBNS is considered a rare condition,1 with a very low estimated incidence of approximately [1]. In 14,000 births [3,4]. BRBNS was first described by Gascoyne in 1860 when he associated vascular hamartomas (nevi) of the skin with vascular intestinal lesions and gastrointestinal bleeding [5]. The term ‘’blue rubber bleb nevus syndrome’’ was coined by Bean a century later [5]. Until 1982, BRBNS lesions were inappropriately named cavernous hemangiomas [2]. Subsequently, vascular tumors were differentiated from vascular malformations based on classification using clinical, radiological, and anatomopathological characteristics. Hemangiomas, which are considered tumors, appear postnatally, grow rapidly due to cellular proliferation, involute later, and have high-velocity flow. In contrast, vascular malformations are present at birth and grow proportionally with the patient. Vascular malformations are further subclassified as capillary, venous, lymphatic, or arterial malformations according to the type of vessels involved, and as slow-flow or fast-flow lesions according to rheology. The three most common syndromic vascular malformations are Klippel-Trenaunay syndrome (capillary-lymphatic-venous malformation with limb hypertrophy), Maffucci syndrome (multiple enchondromas associated with multiple hemangioendotheliomas, with high incidence of malignancy), and BRBNS; the three types of VMs have many findings in common, and therefore, must be considered first in a differential diagnosis. Pathognomonic cutaneous features of BRBNS include small, soft, rubbery, dark-bluish, nipple-like lesions that are easily compressible and refill slowly [2]. VMs of varying sizes and morphologies may be present on the skin and within the GIT [3]. GIT lesions can cause massive or occult gastrointestinal hemorrhage and iron-deficiency anemia secondary to bleeding episodes [6]. Therefore, patients with BRBNS are at greater risk of gastrointestinal bleeding and severe iron-deficiency anemia [2]. Subcutaneous VMs, gastrointestinal bleeding, or refractory anemia are rarely the sole presenting features in patients with BRBNS [2].
A 2-month-old male presented with multiple large, bluish, bleblike, nodular lesions scattered over the face, scalp, neck, trunk, and limbs since birth (Figures 1-4). The nodules were deep blue in color, soft, and 0.5-4.0 cm in diameter. The nodules appeared spherical with a smooth surface, although some exhibited darkred central ulcers. Such large nodules and central ulceration have not been previously reported. The nodules were partially compressible with apparent dermal herniation, refilling slowly upon pressure release. Although the lesions were not painful or tender, occasional bleeding was observed from the ulcers. At a follow up visit months after starting oral propranolol, most of the lesions have considerably regressed, or disappeared- the ulcerated ones leaving a scar behind-, and the child is feeling, and growing well [5].

Figure 1: Multiple large, red nodules on the neck, nose-tip, right lower eyelid, left upper eyelid, forehead, and scalp are evident

Figure 2: The anterior aspect of the right thigh and leg show multiple large, centrally ulcerated nodules

Figure 3: The medial aspect of the right lower limb shows multiple large, centrally ulcerated nodules
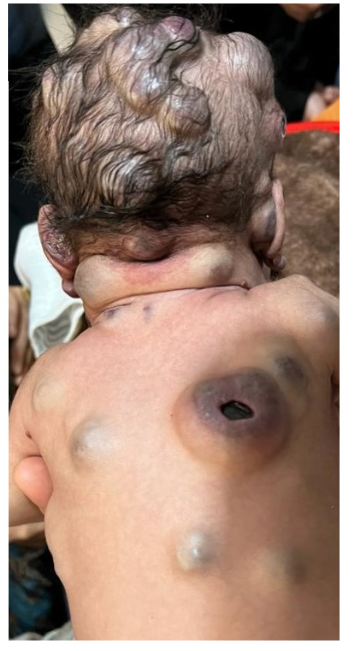
Figure 4: Multiple large, centrally ulcerated nodules on the upper back and confluent intact nodules on the scalp and nape are evident
BRBNS is a rare disorder characterized by cutaneous and GIT VMs [7]. Cutaneous lesions are most frequently seen on the limbs, trunk, and face, 4 which is consistent with our observations in this case. In addition, BRBNS may involve the brain, liver, lungs, and skeletal muscles; this was also observed in our patient’s case (except for the lungs [8]. A meta-analysis conducted by Jin et al,1 on 120 out of 200 BRBNS cases identified from MEDLINE, found that cutaneous VMs were observed in 93% of the cases and gastrointestinal VMs in 76% of the cases; however, these were not evident in our patient’s case. Other sites of involvement included the central nervous system (13%), liver (11%), and muscles (11.9%) 1 all of which were affected in this case.
Complications from VMs can be life-threatening due to the expansion or obstruction of vital structures and associated bleeding. Bleeding from VMs can occur in any affected organ, with variable consequences. In the central nervous system, bleeding can lead to cerebral infarction; bleeding in the liver may lead to hepatopathy; and bleeding within muscles may lead to atrophy, hypertrophy, or dysfunction. In the pharyngeal or laryngeal area, VMs may compromise the airway and lead to snoring or sleep apnea.
In our patient’s case, GIT endoscopy did not indicate GIT involvement. However, computed tomography of the brain, orbit, and chest revealed multiple markedly-enhanced vascular lesions (3-6 mm in diameter) affecting both cerebral hemispheres, and two cystic lesions (22x18 mm and 21x14 mm) in the posterior fossae. The subcutaneous lesions were confirmed; some lesions invaded the muscular tissue, consistent with previous findings [8]. Blood tests indicated signs of normocytic hypochromic anemia, and a white blood cell count of 13.9-14.2 x 109/L was recorded. Negative fecal occult blood test indicated a lack of GIT involvement; this finding was supported by the results of GIT endoscopy. Abdominal ultrasonography revealed a 60x65 mm cystic lesion in the left hepatic lobe. Treatment was started with 5 mg propranolol twice daily. At follow-up,months after treatment initiation, a dramatic response had been achieved; many lesions had regressed with some scar formation [5].
BRBNS should be differentiated from other inherited VMs, such as Osler-Weber-Rendu syndrome, Klippel-Trenaunay syndrome, and Maffucci syndrome, to ensure proper treatment and estimate the prognosis [4]. Osler-Weber-Rendu syndrome is characterized by recurrent epistaxis, positive family history, telangiectasia, and bleeding punctiform angiomas. Maffucci syndrome presents primarily with bone malformations and chondrodysplasia, and secondarily with diffuse skin and soft tissue VMs. Klippel- Trenaunay syndrome is characterized by hypertrophy, deformities of soft tissue and bone, and varicosities, mostly affecting one limb.
This case report is exceptional because of the large number and size of the lesions, the patient’s young age (2-months-old), central ulcerations observed in some lesions, and the rapid response to propranolol. The findings in this case contribute to the knowledge of rare clinical manifestations of BRBNS and can help prevent misdiagnoses, missed diagnoses, and serious complications.
