Author(s): <p>Bala M *, Abubakar AB, Taiwo AO, Abubakar MK, Braimah RO, Isah SA, Ahmad MM, Bawa TA and Jaafaru R</p>
Background: Noma is an infectious disease that rapidly destroys orofacial tissues and neighboring structures in its fulminating course. This study aimed to present a case series of blindness as a result of Noma destruction of the orbital bone and highlight the important aspect of its management.
Patients and methods: This was a case series of 12 patients seen and managed for Noma with associated blindness over 2 years study period at Noma Children Hospital Sokoto, Northwest Nigeria. Sociodemographic variables, presenting complaints, presenting visual acuity, investigations, and, the treatment done was recorded. Data were analyzed using IBM SPSS version 25.
Result: There were 4 (33.3%) males and, 8 (66.7%) females in the age range of 4-15 years with a mean±SD of 7.5±3.3years. The time range of onset before presentation to our facility was 2 weeks to 4 months. Ophthalmic examination revealed a destroyed globe and purulent discharge with no light perception in all the patients. Anemia and malnutrition were present and, microbiological culture and sensitivity (MCS) yielded no growth in all the patients. Patients were optimized, then later had sequestrectomy and, teeth extraction. Monitoring of patients was done until symptoms resolution.
Conclusion: Noma is capable of spreading rapidly to the orbit, causing loss of vision as a complication. However, aggressive medical and surgical intervention in consultation with an ophthalmologist can result in early resolution of symptoms and prevent further spread that may lead to blindness.
Noma also known as Cancrum oris has been defined as a gangrenous disease affecting young children that rapidly destroys the soft and hard tissue of the face leading to a massive loss of substance with obvious esthetics prejudice and functional compromise [1]. Although the etiopathogenesis of noma is not yet fully understood, currently has been linked to an interplay of multiple microorganisms including; Fusobacterium necrophorum, Prevotella intermedia and, Borrelia Vincenti among others [2]. A strong precondition for noma is malnutrition which has been strongly linked to extreme puberty among other factors such as concomitant diseases and poor oral hygiene. Noma begins from simple gingivitis and rapidly progresses to gangrenous stages if not diagnosed early and promptly treated [3]. The resulting gangrene may involve the maxilla and, the mandible, and may extend to the nose and the orbit in an upward spread [4]. Survivors of noma could present with various degrees of facial deformities, trismus or temporomandibular joint ankyloses; resulting in eating problems, oral incontinence, dysphonia and serious psychological problems [5]. Affectation of the eye resulting in loss of vision could even be more devastating to the patient. Vision loss can affect physical health by increasing the risk of falls and quality of life [6,7]. Although several studies have reported the pattern of noma destruction, to the best of our knowledge, this is the first study that aimed at presenting a case series of blindness as a result of Noma destruction of the orbital bone and its contents with a highlight on the important aspect of its management.
This was a case series of 12 patients seen and managed for Noma with associated blindness over 2 years study period (from April 2018 to March 2020) at Noma Children Hospital Sokoto, Northwest Nigeria. Noma children hospital was established in 1999 by the Sokoto State government to provide free services to curtail Noma diseases that became endemic in the study region as well as for research. Sociodemographic variables such as age sex and, patients’ location, were recorded. Also, patients presenting complaints, presenting visual acuity, investigations, and, the treatment done were recorded. Patients with intact vision despite orbital bone destruction were excluded. Data were analyzed using IBM SPSS version 25 (IBM Corp., Armonk, NY, USA).
A total of 12 patients who presented and fulfil the study criteria were recruited in this study amongst which there were 4 (33.3%) males and, 8 (66.7%) females (Figure 1). Patients were in the age range of 4-15 years with a mean±SD of 7.5±3.3years. The time of onset before presentation to our facility was 2 weeks to 4 months. Ophthalmic examination revealed a destroyed globe and purulent discharge with no light perception in all the patients. Anemia and malnutrition were present in both and, microbiological culture and sensitivity (MCS) yielded no growth in all the patients. Patients were optimized, then later had sequestrectomy and, teeth extraction (Table 1). Monitoring of patients was done until symptoms resolved.
|
Cases |
Age |
Sex |
Symptoms duration |
Presenting visual acuity |
Other findings |
Surgical treatment given |
|
Case 1 (Figure 2) |
5 |
M |
1 month |
Nil |
Malnutrition |
Wound debridement + Sequestrectomy |
|
Case 2 |
7 |
F |
2 month |
Nil |
- |
Sequestrectomy + Teeth extraction |
|
Case 3 |
4 |
F |
2 weeks |
Nil |
Malnutrition + Anemia |
|
|
Case 4 |
6 |
F |
9 days |
Nil |
Malnutrition |
Sequestrectomy + Teeth extraction + orbital exenteration |
|
Case 5 (Figure 1) |
9 |
F |
2 months |
Nil |
Malnutrition |
Wound debridement |
|
Case 6 |
12 |
F |
4months |
Nil |
Malnutrition + Anemia |
Wound debridement + Sequestrectomy |
|
Case 7 |
15 |
M |
2 months |
Nil |
- |
Wound debridement + Sequestrectomy |
|
Case 8 |
4 |
M |
7 days |
Nil |
Malnutrition + Anemia |
Wound debridement + Sequestrectomy |
|
Case 9 |
7 |
F |
2 months |
Nil |
Malnutrition |
Sequestrectomy + Teeth extraction |
|
Case 10 (figure 3) |
9 |
F |
2 weeks |
Nil |
Malnutrition |
Sequestrectomy + Teeth extraction |
|
Case 11 |
5 |
M |
12 days |
Nil |
Malnutrition |
Sequestrectomy + Teeth extraction |
|
Case 12 |
7 |
F |
1 month |
Nil |
- |
Sequestrectomy + Teeth extraction |

Figure 1: Clinical picture showing right eye involvement in a female child by the noma disease process

Figure 2: Clinical picture showing right eye involvement in a male child by the noma disease process

Figure 3: Clinical photograph showing left destroyed orbit as part of the noma sequelae

Figure 4 a: Clinical picture showing destroyed left maxilla, nasal cavity, zygoma and, orbit
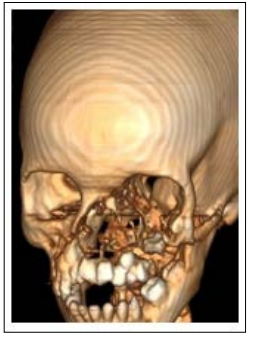
Figure 4b: Computed tomography scan showing destroyed maxilla, nasal cavity, zygoma and, orbit
This study has demonstrated blindness secondary to orbital destruction as one of the unfortunate consequences of late presentation of patients affected by noma. There was female predilection in this series, which agrees with other studies [3,7]. All patients are within the previously reported age of noma occurrence [7,8]. Age and sex may not be an important factor in determining the severity of noma destruction of orbital bone causing blindness.
Noma has been known to progress rapidly and the pattern of spread depends on the initial location of the lesion but upward spread to the nose and orbit was found to be more common [9,10]. The most common site of noma destruction has been the cheek likely because of the nature of the spread of this disease which starts as gingivitis and widens to include the buccal vestibule and hence the cheek and labial mucosa [3]. Noma has been reported to affect mandible, maxilla, temporomandibular region, palatine bone, nasal bone and vomer [11,12]. Bala et al. 4 in a study titled “Clinicopathological analysis of osteomyelitis in noma patients” reported the maxilla as the most commonly affected bone by the noma disease process. Most of the time even with a relatively late presentation, the patient must have died or the disease must have been arrested before the orbital involvement. This series identified cases of orbital destruction causing blindness which indicates the urgency of the need for early intervention.
Orbit houses the eye which is one of the most important sense organs that has the role of vision. Blindness can affect the patient’s physical health and increase the risk of falls and reduce the quality of life [13]. It may also have an impact on mental health. Blindness has also been linked to loneliness, social isolation and, anxiety [14]. This could add to the tendency psychosocial aspect of noma deformity and may increase depression and suicide.
Blindness from infection may result from interference of blood and nutrients supply to the optic nerve, optic nerve compression, or proptosis-induced stretching of the optic nerve [15]. In this series the blindness was due to the destruction of the orbital bone and its contents owing to infection. Although no pathogen was cultured, the mode of transport which does not take into cognizant the anaerobic nature of most odontogenic infectious process might be responsible for this negative result.
The average time of presentation of patients recorded in this series was 2 weeks to 4 months, which indicates the need to establish a highly effective surveillance team in the community for noma detection and early referral.
In this series, patients were managed surgically via wound debridement, sequestrectomy and, teeth extraction. Patients were also supported nutritionally to correct the anemia and malnutrition seen with most of the patients. All patients were monitored until the resolution of the symptoms. The result of this research suggests that these patients could benefit from orbital reconstruction and orbital prosthesis in the future to give complete rehabilitation and better cosmesis.
Reconstruction of orofacial defects due to noma has been quite challenging, especially where composite or complex tissue architecture is lost [16]. Several reconstructive options including local flaps, regional flaps, distant flaps, as well as microvascular flaps have been used to reconstruct the resultant defect in noma survivors each with their merit and demerit, but most of the reported articles concentrated on the soft tissue reconstruction [17]. Apart from these soft tissue defect reconstructions, bone and orbital reconstruction could help in reducing deformity and improving cosmesis [18]. An eye prosthesis could reduce the psychosocial impact of this disease condition.
The present study highlighted Noma as a rapidly spreading gangrenous lesion that could involve the orbit, causing loss of vision as a complication. However, aggressive medical and surgical intervention in consultation with an ophthalmologist can result in early resolution of symptoms and prevent further spread that may lead to blindness. Hence, multidisciplinary approach involving the ophthalmology team is recommended.
Conflict of Interest: None declared
Source of Funding: Nil
