Author(s): Villalba Bachur Roberto*, Spagnuolo Juan Ignacio, Cora Florencia and Longo Emilio Miguel
Human Papilloma virus (HPV) infection is a high incidence entity in the world population. It is highly related to cervical carcinoma, as well as anogenital carcinoma, among others. The presences of bladder HPV lesions are infrequent and there is an association between it and the development of bladder cancer.
Human papilloma virus (HPV) is the main predisposing factor in the cervical carcinoma development. According to the World Health Organization (WHO), it ranks fourth among the most common types of cancer that affect women. In addition, HPV is a predisposing factor for anal, penile, vaginal, urethral, and head and neck cancer development [1]. There are few reports in the literature about bladder compromise due to HPV, especially represented by condyloma acuminatum, characteristic of the infection [2,3]. We present an endovesical HPV clinical case in association with the presence of cervical carcinoma.
A 50 year old woman with a smoking history was diagnosed with stage IIB cervical carcinoma (HPV 11-16) in 2017. An assisted robotic Wherteim Meigs operation was performed, evolving on the first post-surgical day with urinary type debit from drains that was confirmed by analytical studies of abdominal fluid. A bilateral ascending pyelography was performed, showing contrast leakage at the level of the left distal ureter as only finding, and a left percutaneous nephrostomy was placed. 2 months after surgery, a left Taguchi-type ureteroneocystostomy was performed. The patient continued normal oncological controls.
One year after surgery, she consulted referring a single episode of gross hematuria without associated symptoms. In the interview, the patient did not refer a family history of oncological pathologies neither personal pathologies history, she referred smoking habit and a single sexual partner for the last five years. On physical examination, condylomas acuminatum in the perianal region and vulva were evidenced without another positive finding, analytical chemistry in normal parameters except for the presence of 10 red blood cells per field and leukocytosis in the urinary sediment. Negative urine culture. Negative serologies. Ultrasound reported heterogeneous formation at the expense of the bladder floor. In the cystoscopy, two papillomatous formations, pediculated of 0.5 cm and 1 cm, located in the trigonal region and in the bladder neck, near from the uretheral meatus, were evidenced. Ureteroscopy did not show injury to the urinary tract. Holmium laser enucleation of the bladder lesions was performed. It was sent to histopathological study and molecular biology for PCR with suspected HPV, taking into account the previous oncological diagnosis.
The histopathological report showed mucous fragments with squamous epithelium with papillomatosis with basal loss of maturation and frequent mitotic figures, koilocytosis, binucleation, and dyskeratosis, corresponding to low-grade intraepithelial lesion-HPV (Figure: 1).
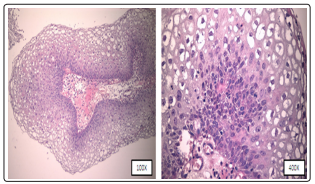
Figure 1: Hematoxylin and eosin (H&E) examination of the bladder biopsy showing papillary growth of squamous epithelium with koilocytosis and nuclear changes characteristic of HPV infection.
The PCR result was HPV injury with presence of genotypes 6 and 11.
Local treatment of perianal and vulvar condylomas was performed with CO2 laser vaporization with good clinical response.
Currently, the patient continues oncological controls with gynecology department without evidence of disease recurrence neither evidence of new HPV lesions. Cystoscopic and cytological controls of urine were performed for one year, every 3 months with negative results.
It is noted that the anonymity is maintained and the written informed consent was obtained from the patient.
HPV is a DNA virus, of the Papilomaviridae family, of double circular chain, not encapsulated, of icosahedral symmetry protein capsid, that reproduces in the nucleus of epithelial cells [4]. HPV infections are of great importance in pre-neoplastic lesions, cervical carcinomas, and other genitals neoplasms [5].
There are approximately 200 HPV genotypes identified, 30 types are responsible for ano-genital infections [6]. Types 16 and 18 are the most frequent genotypes associated with cervical, vulvar, penile and anal cancer, while types 6 and 11 are associated with the development of benign lesions such as warts and condyloma acuminatum (Figure 2) [7].

Figure 2: HPV genotypes classification according to their malignancy potential
There is a lack of scientific evidence in the literature about bladder compromise due to HPV and, therefore, of its relationship with bladder cancer. Gutierrez et al. and Wiwanitkit V et al. Presented two meta-analyzes that showed an increased risk of developing bladder cancer in patients with HPV infection [8,9]. The genotype most associated with the development of bladder cancer is 16 as well as the most prevalent, however low-risk genotypes can also be identified [10].
Na Li et al. suggest a geographic variation in HPV prevalence likely due to genetic background, environmental risk factors, including sexual behavior, smoking, and other ethnic and cultural differences, as well as other unknown sources [10]. Although, condyloma acuminatum is the most common sexually transmitted disease, they occasionally occur in the anterior urethra and in very rare cases are seen in the posterior urethra and bladder [11].
The route of HPV infection is controversial. In our case, it is easy to consider the possibility that the infection was through instruments such as the cystoscope, since the patient previously had external genital lesions, however, its presence can be suspected due to the local extension of her oncological pathology.
On the other hand, so far, there are no literature reports that refer to the follow-up of patients with bladder HPV-DNA positive lesions; regarding cystoscopic controls, diagnostic studies such as ultrasound or urinary cytology, as well as follow-up time. Samarska et al. presented a retrospective study of 31 patients with cases of bladder accumulated condyloma, with an average follow-up of 6 years, reported that in all cases in which associated squamous cell carcinoma was diagnosed, this was performed within the year of first diagnosis [12].
Regarding the treatment performed, most of the works in the literature were treated with mono or bipolar transurethral resection, in our case, we decided to do Holmium laser enucleation due to the size of the tumors, location and quantity, respecting a safety margin. A risky and criticizable procedure was the diagnostic ureteroscopy performed, being able to perform sowings in the upper urinary tract, however, there was no evidence of seeding in the upper urinary tract by imaging or cytological studies.
We highlight the importance of suspecting the etiology of bladder HPV lesions in patients with a previous history of pathologies associated with the virus or anogenital lesions; immunodeficiency is considered as a risk factor for developing bladder injuries. There is an association between bladder HPV and bladder carcinoma, mainly with squamous cell carcinoma. However, more studies are needed on the presence of this bladder pathology and its association with bladder carcinoma, as well as its follow-up, in both high and low-grade lesions.
