Author(s): Arsheed Hussain Hakeem*, Hassaan Javaid, Novfa Iftikhar and Usaamah Javaid
We present a case of reconstruction of a large full thickness cheek defect as a result of cancer ablative surgery. This defect was reconstructed primarily by bi-paddle pectoralis major myo-cutaneous (PMMC) flap. This technique is anatomically sound, technically easy with short learning curve and also reproducible. One has to be careful, not to place more than one third of the skin paddle outside the muscle. This method of reconstruction is an alternative where microvascular free tissue transfer is contraindicated due to medical comorbidity or is not feasible due to either lack of the expertise or infrastructure. It is extremely useful in salvage in cases, in cases of the failure of microvascular flap, in selected large full thickness oral cavity lesions. However, the limitations of this method include loss of nipple area and technical difficulty in females and obese patients.
Full thickness resection of the cheek with loss of mucosa, mandible and cutaneous elements results in extensive defect which is a challenge to reconstruct. To rehabilitate such cases both functionally and aesthetically, one should replace all the tissues lost due to ablative surgery like mucosa, bone and skin. The only flap that can replace all the elements is the osteo-cutaneous fibula microvascular flap [1]. Most of the developed centres will reconstruct such extensive defects with a microvascular free tissue transfer. The limitation of reconstruction with free flaps in developing countries is that it cannot be performed in all cases as the expertise and infrastructure is not available in all centres. Such flaps need long operative time and centres with the large work volume, particularly in developing countries, cannot offer it to all patients [2]. One more scenario, where it is not possible to use free flaps is in the setting of salvage reconstruction, if free flap has failed due any reason. Other options for reconstruction of such complex full thickness cheek defects is double flaps like PMMC flap for inner lining and deltopectoral flap for outer covering. Reconstruction with double flaps like these comes at the cost of increased morbidity. Since this is a robust pedicle flap, it can with stand adjuvant radiotherapy also.
We describe step by step technique of bi-paddling the PMMC flap and use it in reconstruction of such complex full thickness cheek defect. Since there is no standard method to bi-paddle the PMMC flap so that vascularity to both the paddles is preserved, folded PMMC flap without making two paddles has been described for such defects both for inner lining as well as outer cover [3]. Circulatory disorders may exist in 12-19% cases of PMMC flaps, therefore surgeons prefer folded flaps over paddling [4]. We adopted the method of bi-paddling of PMMC as described by Ahmed GQ et al for large full thickness defects of oral cavity [2]. Total operative time for composite resection and reconstruction varies from 3.5 to 4 hours depending on the expertise of the surgeon. A step by step approach for the bi-paddling the PMMC flap for large full thickness defects of oral cavity with representative clinical pictures is presented to help surgeons to rehabilitate such cases.
On the basis of the size of full thickness cheek defect (Figure 1A) resulting from the cancer ablative surgery, the skin paddle is designed horizontally around the nipple and areola (Figure 1B). The medial extend is from midline and the lateral border of the skin can cross the lateral border of pectoralis major muscle. The medial paddle is designed medial to the nipple areola complex and will be used to reconstruct the outer skin defect, while the lateral paddle is designed around the nipple for reconstruction of the mucosal lining (Figure 1B). Placing the paddle horizontally has advantage of reaching the desired place of buccal mucosa without compromise of the length. We prefer to make lateral incision first along the lateral edge of the pectoralis major muscle and expose it (Figure 1C). This also allows to confirm the placement of the skin paddle over the pectoralis major muscle by direct visualization. After confirming the position of the flap, we make the upper incision first and raise the upper chest wall to make a subcutaneous tunnel for the passage of the flap (Figure 1C). The chest wall subcutaneous flap and the subplatysmal neck skin flaps are connected over the clavicle so that at least four fingers can be passed to allow the passage of the pectoralis major myo-cutaneous flap comfortably without compression of the vascular pedicle (Figure 1D). We prefer to separate the pectoralis major muscle from the pectoralis minor muscle on the chest wall with blunt finger dissection and visualize the vascular pedicle (Figure 2A). This is avascular plane between the pectoralis major and pectoralis minor muscles (Figure 2A). We prefer not to make inferior incision over skin paddle till the thoraco-acromial vascular pedicle is completely identified, which is seen running on the under surface of the pectoralis major muscle (Figure 2A). Only after identifying of the thoraco-acromial vascular pedicle, incision is made on the inferior border of the designed skin paddle and deepened and lifted along with the muscle without separating the two paddles (Figure 2B). We cut and separate the pectoralis major muscle laterally (Figure 2C) and medially with care taken to be away for the vascular pedicle till the clavicle bone is reached (Figure 2D). Skin paddle may or may not be secured to the muscle with few chromic catgut sutures to avoid shearing of perforators depending on expertise of the surgeon. It is advisable for the beginners to secure the skin paddle to muscle with few sutures. With sharp dissection, the muscle is elevated from the ribs and medial pectoral nerve may be cut with scissors to avoid compression of vessels after the flap is transposed over the clavicle (Figure 2D). The flap is then transposed over the clavicle to the donor site defect under the chest subcutaneous and neck subplatysmal flaps (Figure 3A and B). We prefer to divide the cutaneous part of the flap into two paddles after it is transferred to the recipient site (Figure 3C). The lateral paddle bearing the nipple and areola is inset first to reconstruct the inner mucosal defect (Figure 3D) and the medial paddle is used for reconstruction of the outer skin defect (Figure 4A). Before closure of the chest wall the thoraco-acromial vascular pedicle is again examined to see if it is comfortably placed without compression. Primary closure of the chest wall donor site is usually possible, despite the large size of the skin paddle, due to the wide undermining of skin flaps (Figure 4B). Closed suction drains are used to drain the donor site as well as the neck
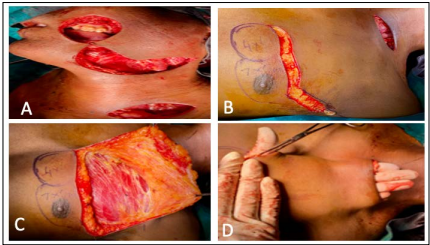
Figure 1 (A): Full thickness Cheek defect as a result of Cancer Ablative Composite Resection;
Figure 1 (B): Design of Bi-Paddle Skin Flap Horizontally around the Nipple area;
Figure 1 (C): Lateral Incision along the Lateral Border of the Pectoralis Major Muscle and raising Upper Chest wall Flap up to the Clavicle;
Figure 1 (D): Subcutaneous Tunnel over the Clavicle for the Passage of PMMC flap should allow passage of 4 fingers.
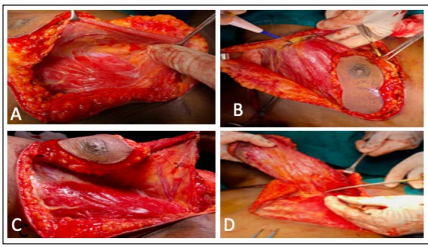
Figure 2 (A): Separation of the Pectoralis Major Muscle from the Pectoralis Minor with identification of the Avascular Plane between Pectoralis Major and the Thoraco- Acromial Vascular Pedicle;
Figure 2 (B): Division of the Pectoralis Muscle laterally;
Figure 2 (C): Preservation of the Thoraco-Acromial Vessels;
Figure 2 (D): Complete division of the Pectoralis Major Muscle Medially and laterally up to the Clavicle and careful division of the Medial Pectoral Nerve.
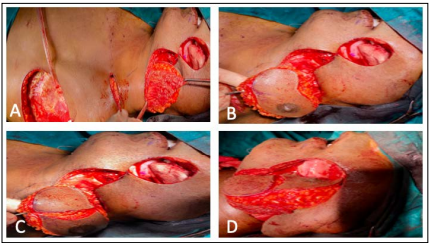
Figure 3. A and B: Passage of the pectoralis major myo-cutaneous flap below the subcutaneous tunnel without division into paddles;
Figure 3 (C): Division of the skin into two paddles after transposition to the neck;
Figure 3 (D): Inset of the lateral paddle with nipple for inner mucosal lining

Figure 4 (A): Medial paddle used to reconstruct the outer skin defect;
Figure 4 (B): Primary closure of the chest wall.
This pictorial assay demonstrates step wise elevation of the bipaddle pectoralis major flap for reconstruction of full thickness cheek defect. This technique is useful in patients where microvascular free flaps are not feasible either due to nonavailability of expertise and infrastructure or comorbidity. It is also playing an important role in cases were the free flaps have failed due to any reason. It has short learning curve and is reproducible technique. It is robust flap which can with stand adjuvant radiation therapy also.
