Author(s): Boccaccio S
Glossopharyngeal neuralgia is a rare condition that occurs far less than other cranial neuralgias, such as trigeminal neuralgia. Glossopharyngeal neuralgia, due to its location, diagnosis is often difficult. Numerous diagnoses contribute to the differential, especially, when the patient arrives with acute facial pain. Our patient arrived in our rehabilitation department suffering from atypical neck and facial pain.
The neuropathic facial pain leading to a significant deterioration in quality of life. We can distinguish two types of neuropathic pain, episodic neuropathic pain, including trigeminal or glossopharyngeal neuralgia, characterized by paroxysmal episodes of short duration, and continuous neuropathic pain as in peripheral neuritis, or post herpetic neuralgia in which the pain is more constant.
Glossopharyngeal neuralgia is a rare disorder characterized by recurrent attacks of severe pain in the posterior pharynx, tonsils, back of the tongue, middle ear, and below the angle of the jaw.
Because of this location, clinical features and rarity, the diagnosis is often difficult and confused as trigeminal neuralgia.
It is a rare disease, with an incidence rate of 0.7 cases per 100,000 inhabitants. It is more common in patients over the age of 50. It occurs equally in both males and females and is often seen on the left side [1].
In 74% was reported a spontaneous remission. 88% of patients reported unilateral pain, while the other 12% had bilateral pain in the sensory distribution of the glossopharyngeal nerve.
Interested patients who are 50 years old and older. There is a higher incidence in females affected by pain in the neck regions; therefore, both men and women are equally affected.
Pain attacks are one-sided, short-lived, and occur spontaneously. The affected area includes the mastoid, back of the throat, and the tongue, back of the nose, Eustachian tube and middle ear, tonsils. Patients may have difficulty speaking and swallowing.
The pathology is idiopathic, but vascular compression of the ninth cranial nerve, as well as oropharyngeal neoplasms, peritonsillar infections, and other lesions, have been described.
The attack persists for less than seconds to 2 minutes, and patients can experience 30 to 40 attacks in one day.
The diagnosis is clinical. MRI can rule out tumor or vascular abnormality, and MR angiogram may rule out vascular compression in the posterior inferior cerebellar artery. An X-ray will diagnose whether Eagle syndrome is the cause.
Several diagnoses contribute to the differential, including trigeminal neuralgia, geniculate neuralgia, and atypical pain syndrome, but most cases of glossopharyngeal neuralgia are idiopathic in which no identifiable lesion can be discovered [2].
A 58-year-old patient comes to our rehabilitation department. He suffers from pancreatic cancer and for six months, he has been reporting severe neck pain, spontaneous or stimulated by chewing or swallowing.
The painful attack for a few minutes begins at the base of the tongue, radiates to the ipsilateral ear, extends to the posterior neck in the cervical area, and the frequency during the last few weeks seems to increase, especially during the night.
He arrives with a diagnosis of neck pain in cervical spondylosis, manifests anxiety, insomnia, and takes steroids and non-steroidal drugs, but with poor results.
Allodynia and hyperalgesia were present on the left side of the neck, extending from the ipsilateral ear to the upper edge of the trapezius.
For examination, we used a numeric number scale (n.r.s.) for pain and a goniometer for articular range of motion.
Neck examination showed decreased range of motion (20 degrees), especially in right latero-flexion, pain contractures of the cervical paravertebral muscles, (n.r.s. 8/10), shoulder elevation and abduction deficits (90 degrees). Compression of the great occipital nerve caused severe pain (n.r.s. 10/10)
On palpation, on the left side of the neck in the medial part of the sternocleidomastoid muscle, there was an area similar to hard rubber band, very painful.
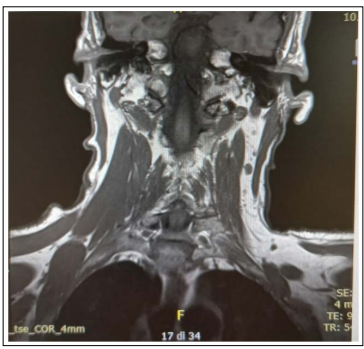
An ultrasound revealed a hyperechoic area that an MRI missed, but indicated the presence of lymph nodes on the lateral side of the neck (see Figure 1).
We requested a CT scan to study the styloid process, to rule out Eagle syndrome. The CT scan showed a normal appearance of this.
When our patient arrives, he was suffering from a complex pain syndrome. Neck pain was very noticeable aching (n.r.s. 8/10), such as large occipital nerve, paravertebral muscles contracted, and left shoulder defective.
He showed neuropathic symptoms at the base of her tongue, radiating into her ear and below the angle of her jaw. Rushton et al in 1981 demonstrated that an anesthetic can be applied topically, which can be both diagnostic and therapeutic for glossopharyngeal neuralgia [3].
Based on this study, we applied an intradermal infiltration of 2% lidocaine in the medial area of the sternocleidomastoid muscle, in the area of hyperalgesia, and noted a pain reduction for 48 hours (nr 4/10)
Based on this result, we started treatment with carbamazepine and pregabalin [4].
Several studies show that carbamazepine aided pain relief in glossopharyngeal neuralgia symptoms, and in a case study of a woman, gabapentin therapy actually stopped her symptoms, with no side effects to the drug.
The treatment plan was carbamazepine 400 mg and pregabalin 75 mg twice daily In addition, for pain we used tapentatol 100mg twice a day.
After one week, we noted a reduction in the intensity and number of pain attacks especially during the night, and an improvement in allodynia and hyperalgesia in the areas affected by neuralgia (n.r.s. 4/10), a decrease of anxiety and insomnia.
The contractures of paravertebral muscles were reduced and we note an increase of range of motion of cervical in all plans of range of motion, and shoulder (120° in elevation and adduction)
We had planned a local treatment of the greater occipital nerve with lidocaine 2% and triamcinolone, but the results did not make it necessary
Glossopharyngeal neuralgia is a painful and extremely rare syndrome that produces pain in an area including the ear, base of the tongue, throat, tonsillar fossa and angle of the jaw.
Diagnosis is difficult due to its location, clinical features and rarity. Our patient presented with a complex pain syndrome characterized by neck pain, involvement of the occipital nerve and the glossopharyngeal nerve.
Intradermal treatment with 2% lidocaine in the area affected by allodynia and hyperalgesia corresponding to the distribution of the glossopharyngeal nerve was important for the diagnosis. Treatment with carbamazepine and pregabalin resulted in pain relief with reduction in the number and intensity of attacks.
