Author(s): Singh Kriti*, Nigam Seema and Tripathi Saurabh
Introduction: Health care providers are working round the clock in their fight against COVID-19. Appropriate measures are taken by the hospital administration and also healthcare providers for the protection of patients as well as for them. This study is taken up to assess infection risk of COVID-19 among healthcare providers about infection, prevention, and practices in a tertiary healthcare facility.
Health care providers are working round the clock in the fight against COVID-19 pandemic. Infection risk is high among the frontline workers as they are exposed to the virus continuously for longer periods. Appropriate measures are taken by the hospital administration and also healthcare providers for the protection of patients as well for them. The virus that causes COVID -19 was initially called as 2019-nCoVand was then termed as syndrome coronavirus 2 (SARS-CoV-2) by the International Committee on Taxonomy of Viruses (ICTV) [1].
Previously, the severe acute respiratory syndrome-coronavirus (SARS-CoV) and the Middle East respiratory syndromecoronavirus (MERS-CoV) have been known to affect humans. Outbreaks of respiratory disease caused by these viruses seem to have originated in animals before moving into other hosts like humans. MERS-CoV was found to be transmitted from Arabian camels to humans, whereas SARS-CoV was transmitted from civet cats to humans. SARS-CoV-2 seems to have originated from bats and first reports of cases were from Wuhan, Hubei Province in China, suggesting an animal-to-person spread from a live animal market. The virus then spread outside Hubei and subsequently, to the rest of the world via human transmission. Several countries have now reported community spread. The World Health Organization (WHO) declared coronavirus disease as a pandemic on March 11, 2020 [2].WHO defines health workers as ?all people engaged in actions whose primary intent is to enhance health? [3].This usually includes doctors, nurses, paramedical staff midwives, community workers, hospital administrators their support staff. Mainly all personnel working in core clinical services, supportive functions or are in training serving on the frontlines to curb the infection of COVID-19.In India, according to the Indian Council of Medicine Research, 5.2% of the COVID-19 infected patients are healthcare workers [4]. They all are now facing it as an occupational risk. It is leading to the detrimental impacts on their own lives patients, health system functioning and their families.
The emergency response to COVID-19 around the world has also highlighted the major impact of healthcare worker safety. Reports estimate that in February 2020, there was a total 500,000 medical staff in Hubei province, the epicenter of COVID-19 outbreak, with many doctors working 24-hour shifts while the outbreak rapidly expanded in the area.The PPE shortage has forced healthcare workers to fashion protective equipment from garbage bags, raincoats, and plastic file bags [5]. Infections among healthcare workers may also indirectly impact their job attendance and retention due to additional fear and stigma of working in high-risk environments.A total of 288 healthcare workers had been infected, increasing the fear of many healthcare workers to return to work. This added to the already ??rapid breakdown of essential health services, with consequent ramifications for endemic infectious diseases and noncommunicable disease-related care, such as diabetes and maternal health [6].A meta-analysis of 59 outbreaks (including SARS, MERS, influenza, and COVID-19) found that staff in contact with affected patients had nearly twice the levels of both acute or post-traumatic stress and psychological distress than did lower risk controls, with the primary risk factors for psychological distress including younger age, junior status, being parents of dependent children, or having an infected family member [7]. Risk determinants to healthcare workforce safety represent potential points of failure in the effort to limit and control The identification of specific determinants for a particular diseaseboth within the health system and during an emergency-is the first step to mitigating risk of exposure. Although not always possible, especially in the case of a novel pathogen, some measures to address determinants common to past disease outbreaks can be applied generally to improve epidemic preparedness and control [6]. This study was taken up to assess infection risk of COVID-19 among healthcare providers about infection prevention control and practices in a tertiary healthcare facility.Absent /On leave and not willing to participate in the study.
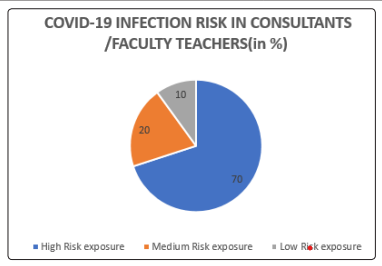
A survey was conducted at a tertiary-care hospital and teaching institute GSVM Medical College and Lala Lajpat Rai Hospital. The survey was prepared in the form of an online form using the Google Forms applications. Printed handouts were also used to cover the potential subjects. The survey covered a total of 242 subjects. The responders included 60 consultants,64 resident doctors,68 nursing staff workers, and 50 class IV workers working as the frontline workers in COVID-19 pandemic in the COVID duty. The period of the survey was of 2 months from 4th October to 4th December, 2020and a total of 242 responders completed the survey. The self-administered questionnaire consisting of socio-demographic questions, and questions based on risk assessment and management of exposure of healthcare workers in the context of COVID-19, the current interim guidance published by the WHO, updated on March 19th, 2020.Consent was obtained by all participants in this study. Convenient sampling method was used for data collection, and the distribution of responses was presented as frequency and percentages. Scores were calculated for the four groups of health care providers and risk of infection was graded as mild, moderate, significant and severe. Data was collected & tabulated on MS Excel sheet & results were drawn using SPSS 27 Version.| GRADE OF INFECTION RISK | NO. OF CONSULTANTS (n=60) | PERCENTAGE OF CONSULTANTS |
|---|---|---|
| High Risk exposure | 6 | 10 |
| Medium Risk exposure | 18 | 30 |
| Low Risk exposure | 36 | 60 |
| Total | 60 |
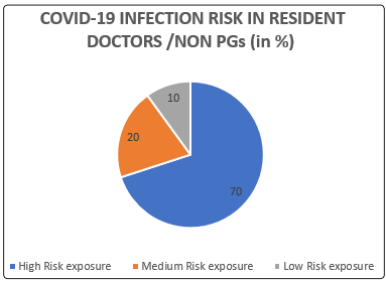
| GRADE OF INFECTION RISK | NO. OF RESIDENT DOCTORS (n=65) | PERCENTAGE OF RESIDENT DOCTORS |
|---|---|---|
| High Risk exposure | 20 | 30 |
| Medium Risk exposure | 32 | 50 |
| Low Risk exposure | 13 | 20 |
| Total | 65 |
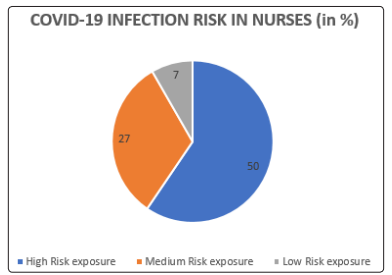
| GRADE OF INFECTION RISK | NO. OF NURSES (n=68) | PERCENTAGE OF NURSES |
|---|---|---|
| High Risk exposure | 34 | 50 |
| Medium Risk exposure | 27 | 27 |
| Low Risk exposure | 7 | 7 |
| Total | 68 |
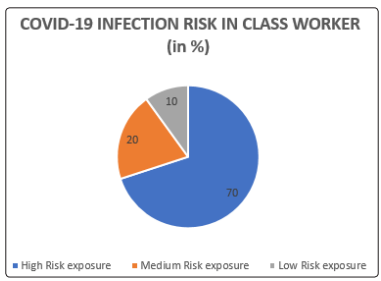
| GRADE OF INFECTION RISK | NO. OF CLASS IV WORKERS (n=50) | PERCENTAGE OF CLASS IV WORKERS |
|---|---|---|
| High Risk exposure | 35 | 70 |
| Medium Risk exposure | 10 | 20 |
| Low Risk exposure | 5 | 10 |
| Total | 50 |
| COVID-19 INFECTION RISK SCORES | MEAN | STANDARD DEVIATION |
|---|---|---|
| OVERALL RISK SCORE | 15.64 | 8.04 |
| CONSULTANTS RISK SCORE | 10.73 | 6.10 |
| RESIDENT DOCTORS RISK SCORE | 13.73 | 7.33 |
| NURSE RISK SCORE | 21.33 | 6.42 |
| CLASS IV WORKER RISK SCORES | 16.77 | 8.35 |
| Exposure category | Circumstances | Recommended monitoring |
|---|---|---|
| High-risk exposure | HW who has assisted a COVID-19 case and performed procedures that generate aerosols or manipulated biological samples during which direct exposure of the skin or mucous membranes occurred without adequate PPE. | Stop all health care interaction with patients and get tested for COVID-19; Quarantine and daily self-monitoring of temperature and respiratory symptoms for 14 days after the last day of exposure to a COVID-19 patient. |
| Medium-risk exposure | HW who had prolonged close contact with patients with COVID-19 not equipped with the indicated PPE without direct exposure to the patient?s biological materials or in the event of noncompliance with the procedures indicated. | Daily selfmonitoring of temperature and respiratory symptoms for 14 days after the last day of exposure to a COVID-19 patient and weekly active surveillance |
| Low-risk exposures | HW who has assisted the case or manipulated biological samples, with the indicated PPE, and without accidents or episodes discordant with the indicated procedures. | Daily self-monitor of temperature and respiratory symptoms for 14 days after the last day of exposure to a COVID-19 patient and weekly active surveillance. |
Our study found that there is a low risk among the consultants (60%), residents and nursing staff faces a medium infection risk of 50 % each and the class IV workers were having a very high risk of infection. It determined the risk of infection among healthcare workers using the there knowledge regarding the infection prevention and control practices. Bandyopadhyay S studied infection and mortality of healthcare workers worldwide from COVID-19. The study was a systemic review [10]. A total of 152 888 infections and 1413 deaths were reported. Infections were mainly in women (71.6%, n=14 058) and nurses (38.6%, n=10 706). Europe had the highest absolute numbers of reported infections (119 628) and deaths (712), but the Eastern Mediterranean region had the highest number of reported deaths per 100 infections (5.7). Our study studied a very small section of population in a localized area. The sample size needs to be from varied healthcare facility to draw any conclusions [9].
Modi et al conducted a study on COVID-19 awareness among healthcare students and professionals in Mumbai Metropolitan Region [11] . The study was a questionnaire-based survey. The overall awareness for all subgroups was adequate with 71.2% reporting correct answers. The highest percentage of correct responses were from undergraduate medical students and the lowest was from non-clinical/administrative staff. Less than half of the total respondents could correctly define ?close contact.? More than three-fourths of the responders were aware of the various infection control measures like rapid triage, respiratory hygiene, and cough etiquette and having a separate, well ventilated waiting area for suspected COVID-19 patients. However, only 45.4% of the responders were aware of the correct sequence for the application of a mask/respirator, and only 52.5% of the responders were aware of the preferred hand hygiene method for visibly soiled hands. Whereas our study tried to cover the professionals working in the taskforce round the clock and not trainees. Our study gives an insight into the real-world problems associated to the current scenario. Yamini, et al conducted a study on Perception and practice regarding infection control measures among HCWs in the district hospitals of Mangalore, India [12]. The study included 120 participants al healthcare workers The study found out that majority (85.8%) was aware of disposing used needles and syringes in punctureresistant containers but only 55.7% were actually practicing it. Three-fourths (75.8%) of the participants were aware about not recapping the needles after use but on observation, only 35.4% were practicing this. All healthcare workers were aware about the indication for using masks and gloves while handling patients, while only 77.1% were using them. We also found that only 61.8% washed their hands after attending every patient, 94.3% cleaned the area with a sterile swab before giving injections and only 35.7% of the labs/ wards/ operation theatres had three colored bags. Our study also calculated the mean infection risk scores among HCWs by categorizing their scores in three categories low-risk exposure, medium risk exposure and highrisk exposure groups. Individual question response assessment was avoided and an cumulative risk assessment by scoring was taken as basis to assess the infection risk among HCWs.A survey was conducted on 60 consultants, 64 resident doctors, 68 nursing staff workers, and 50 class IV workers working as the frontline workers in COVID-19 pandemic. A predesigned and pretested questionnaire was self-administered to the healthcare personals. Data was collected, analyzed and conclusions were drawn. The following were the observations.
The overall mean infection risk score among healthcare providers was found to be high-risk exposure in nurses and low risk exposures in consultants. The risk score was found to be in medium risk exposure among residents and class IV workers. The consultants or the senior faculty doctors were exposed to a low risk of exposure as they were mainly in administrative, monitoring and evaluation related tasks. The group of junior doctors and nurses were in medium risk. The teaching sessions and seminars on COVID-19 infection management has put them in medium risk as there are more aware despite the high exposure with patients. Class IV workers are concluded to be at the highest risk as they have the highest exposure and lack proper awareness and therefore high at the risk of contracting and spreading the infection. Risk mitigation strategies, including infection prevention and control (IPC) practices, are meant to keep healthcare workers safe from occupational exposure to disease and to protect patients from healthcare-associated infections (otherwise known as healthcare-acquired infections). Despite ongoing IPC efforts, steady rates of both healthcare associated and healthcare worker infections signal that these mitigation measures have been inadequate at all levels. The lack of both basic IPC and disease-specific training, including necessary reinforcement and supervised practice over time, are determinants of risk for healthcare worker safety. These trainings help healthcare workers recognize, and respond effectively to, patients that may expose a high risk of infection-even in settings outside of their formal place of work.