Author(s): Aynnara Soares Barbosa, Elita Oliveira Da Silva, Jordana Maria Monte Torres and Antonione Santos Bezerra Pinto*
Bipolar Disorder (BD) is characterized by chronic and complex disturbances, featuring periods of depression and phases of mania or hypomania. Considering the studies already conducted, it is important to highlight the efficacy of lithium in individuals, especially in relapse prophylaxis, acute mani a phases, and suicide prevention. Thus, this article aims to address various aspects related to the intrinsic relationship between Bipolar Disorder and the use of lithium, specifically for the maintenance therapy of this condition; to explore the mechanism of action of lithium, demonstrating the benefits of this therapy so that professionals and students in the field can gain a clearer understanding of the subject and evaluate the effectiveness of continuous lithium particle use in treatment. This work is based on a literature review conducted on the Pubmed and Scielo databases from 2018 to 2023. The descriptors used were lithium, treatment, and bipolar disorder. In this context, the review of studies on lithium is essential for healthcare proof essionals and the families of individuals to understand the importance of this substance in maintaining mood stability in patients.
Bipolar Disorder (BD) is an illness that traces its discovery back to Araeteus of Cappadocia, a resident of Alexandria in the 1st century AD, who established a connection between mania and melancholia. Subsequently, the French psychiatrist/neurologist Jules Baillarger described a new form of insanity, termed “la folie a double forme “ (dual form of insanity), characterized by episodes of both mania and depression within the same patient. This disorder is marked by chronic and complex disturbances involving periods of depression and phases of mania and hypomania. These phases alternate with periods of remission and are associated with specific cognitive, physical, and behavioral symptoms [1].
Depressive episodes in bipolar disorder are classified as mild, moderate, or severe. Consequently, the distinction between unipolar depression and depression related to bipolar disorder is crucial for guiding appropriate treatment in each case. However, distinguishing them based solely on presented symptoms is not feasible; it is necessary to consider clinical characteristics such as family history, symptom profile, and the course of the disease in each individual. Many individuals exhibit multiple depressive episodes before the occurrence of the first mani a or hypomania episode [2].
In 1986, lithium was introduced in medicine for the treatment of gout, and for years, it has been used as an antiepileptic and general tonic, with lithium bromide serving as a hypnotic. Lithium, a chemical element with the symbol Li, atomic number 3, and atomic mass 7, belongs to Group 1 (Family 1A) and is an alkali metal. Today, lithium is characterized as the gold standard for bipolar disorder treatment, as it reduces manic and depressive episodes and suicidal tendencies, proving highly effective in bipolar disorder prophylaxis. However, its mechanism of action is not yet fully understood. It is known that this substance bears a resemblance to sodium and can induce changes in catecholamine metabolism. With such similarity, it alters charge transport without active transport through the sodium potassium pump, avoiding energy expenditure, potentially elevating serotonin levels and reducing noradrenaline levels, consequently affecting dopamine, GABA, and acetylcholine concentrations [3].
In this context, lithium acts on Norepinephrine (NE), increasing the metabolic activity of brain amines and the reuptake of NE in synaptic clefts, reducing NE release. Lithium also acts on glycogen synthase kinase Lithium also acts on glycogen synthase kinase-- 33β (β (GSKGSK--33β) β) enzymes found abundantly enzymes found abundantly in the central nervous system, promoting the phosphorylation of substrates that ensure the in the central nervous system, promoting the phosphorylation of substrates that ensure the homeostasis of various biological processes. Considering this correlation, this arhomeostasis of various biological processes. Considering this correlation, this article aims ticle aims to emphasize the importance of this medication for maintaining patients with Bipolar to emphasize the importance of this medication for maintaining patients with Bipolar Disorder. It details aspects of the substance, such as its side effects when in contact with Disorder. It details aspects of the substance, such as its side effects when in contact with the human body, themechanism of action, and the long the human body, the mechanism of action, and the long-term benefitsterm benefits and efficacy of and efficacy of continuous use of this particle, intending to enhance the understanding of professionals continuous use of this particle, intending to enhance the understanding of professionals and students in the field through the analysis of recent studies and students in the field through the analysis of recent studies [4].
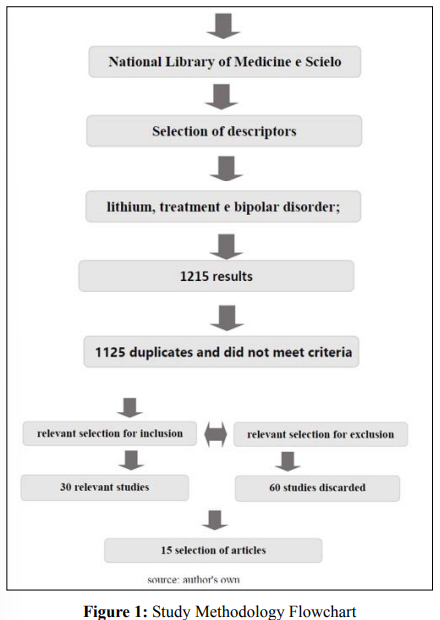
This study adopts an integrative literature review approach. The study design comprises the following stages: selection of databases and choice of descriptors for data filtering, formulation of inclusion and exclusion criteria for articles in this study, and selection of articles coherent with the theme to validate the study’s objectives (Figure 01).
In this context, the research tools used for the literature review were digital articles, primarily from the National Library of Medicine (PubMed) and Scielo databases. The article’s development was based on preliminary analysis studies, with the descriptors being: Lithium, Treatment, Bipolar Disorder.
For this purpose, articles published between 2018 and 2023, in Portuguese and English, were included. Only studies available in full, free of charge, and directly related to the importance of lithium for treatment were considered. Research with publication dates exceeding the last 6 years, provided as abstracts, or with inconclusive methodologies were excluded.
Combining the PubMed and Scielo databases yielded a total of 1215 articles. After reviewing the titles of the articles, it was observed that some articles were duplicates across databases, and others did not meet the criteria for this study. Consequently, 30 articles were selected for further reading, while 60 articles were discarded due to their incompatibility with the purpose of this study. Through this careful analysis, a final selection of 15 articles, comprising literature reviews that initially met the review criteria, was obtained.
Bipolar Disorder (BD), also known as “Bipolar Affective Disorder,” is a psychiatric condition marked by intense mood swings within an individual, navigating between the two opposing poles of affectivity. Additionally, the activities of the affected individ ual are significantly disrupted, with the disease manifesting as either an elevation of mood and increased energy and activity (mania or hypomania) or a lowering of mood and decreased energy and activity (depression) [5].
According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM 5), the disorder is classified into two main types: Type I, where mood elevation is severe and persistent (mania), and Type II, where mood elevation is milder (hypomania). The specifier “with mixed features” is applied to states where there is concurrent occurrence of manic and depressive symptoms, although these are traditionally viewed as opposite poles of mood [6].
There is suspicion that Bipolar Affective Disorder partly arises from a malfunction of the circadian system, given that mood stabilizers are considered chronobiological agents, as noted by Dallaspezia and Benedetti. This becomes particularly relevant in th e disorder’s pathogenesis, especially when discussing the inadequate secretion of melatonin, a hormone produced by the pineal gland that aids in maintaining the sleep wake cycle. Its secretion is controlled by the suprachiasmatic nucleus, which receives inf ormation about environmental light levels through the retinohypothalamic tract in individuals with BD. During manic episodes, there is an increase in the secretion of this hormone, and the peak secretion occurs earlier than expected. In episodes of depress ion and during euthymic periods, the secretion pattern differs [7].
Furthermore, serum levels of melatonin in individuals with Bipolar Disorder (BD) are lower than those in healthy individuals, regardless of their current mood state. Additionally, they exhibit an exaggerated response from the pineal gland to light stimulation compared to individuals without BD [8].
The goal of treating the disorder is to reduce the duration and intensity of acute mood swings and prevent the recurrence of new episodes. In this context, lithium remains the gold standard for bipolar therapies and is still widely used, despite recent advances in the field and the increased use of specific antipsychotics and antiepileptics [9].
Lithium is a chemical element with an atomic number of 3, represented by the symbol ‘Li.’ Belonging to the alkali metal group, it is the lightest metal and the least dense solid element. Lithium carbonate is often prescribed as a mood stabilizer,particularly in the treatment of aggressive impulsive behaviors and primarily in bipolar disorders. It is an inorganic salt composed of two lithium cations (Li+ ) and one carbonate anion (Li 2 CO 3 ). Lithium acts on multiple neurological circuits, causing an increase in the concentration, synthesis, and turnover of acetylcholine in the cholinergic system and a decrease in the concentration, storage, and release of dopamine and norepinephrine in the catecholaminergic system [10].
The mechanism of action of lithium is complex and not fully understood, with a myriad of effects on different cellular pathways and biological systems. These include the inhibition of inositol monophosphatase (IMPA) and glycogen synthase kinase 3 beta (GSK 3 beta), as well as various effects on neurotrophic factors, neurotransmitters, mitochondrial respiration and oxidative metabolism, apoptosis, neuronal and glial structures, second messenger systems, and biological systems such as the circadian rhythm and the hypothalamus pituitary adrenal axis [11].
Moreover, it is noteworthy that mitochondrial dysfunction and abnormal cerebral energy metabolism have been implicated as key aspects of the pathophysiology of bipolar disorder through multiple lines of evidence from imaging, gene expression, and cellular studies. Several studies have confirmed reduced cerebral concentrations of N-acetyl aspartate (NAA) in patients with bipolar disorder. NAA is the second most abundant amino acid in the central nervous system after glutamate, synthesized by mitochondria, and its decreased levels may indicate impaired mitochondrial energy production. Recent studies have demonstrated that chronic lithium treatment resulted in high levels of studies have demonstrated that chronic lithium treatment resulted in high levels of phosphorylation of cytoskeletal and mitochondrial proteins in synaptoneurosome phosphorylation of cytoskeletal and mitochondrial proteins in synaptoneurosome preparations from the prefrontal cortex of rats. Additionally, these studies proposed that preparations from the prefrontal cortex of rats. Additionally, these studies proposed that ththis alkali metal regulates both mitochondrial migration and energy production, positively is alkali metal regulates both mitochondrial migration and energy production, positively influencing the expression of various genes related to mitochondria, including COX5A, influencing the expression of various genes related to mitochondria, including COX5A, NDUFS7, NDUFAB1, in the frontal cortex of mice [11]. NDUFS7, NDUFAB1, in the frontal cortex of mice [11].
Since the 1970s, lithium has been prescribed for bipolar therapies and is still widely used, despite advances in the use of specific antipsychotics and antiepileptics. It remains the first choice for treatment, demonstrating efficacy in the treatment of schizophrenia, as well as various phases of bipolar disorders, including mania, hypomania, and impulsivity. Lithium contributes to prev enting suicidal behaviors in patients with bipolar or major depressive disorder [3].
The specific biochemical mechanism of lithium’s action in mania is unknown. Theoretically, unlike other psychoactive drugs, it does not have a psychotropic effect on normal individuals at therapeutic concentrations. However, the use of this treatment requires knowledge and analysis of factors crucial for ensuring its beneficial effects, as it is excreted by the kidneys. Therefore, it is essential to perform biannual tests of renal function, including urea and creatinine levels, as well as thyroid function and calcium levels, to detect any potential failure that could lead to lithium accumulation and toxicity [12].
Adverse reactions to lithium vary widely, ranging from mild or clinically irrelevant reactions to more severe outcomes, such as hospitalization, impairment, or death. The most commonly mentioned side effect is “intoxication syndrome,” a set of symptoms that can affect individuals through the central nervous, gastrointestinal, renal, and cardiovascular systems. Neurological symptoms include an altered state of consciousness, cerebellar changes leading to tremors, dysarthria, ataxia, and nystagmus, while extrapyramidal and neuromuscular symptoms may manifest as fasciculations, myoclonus, and polyneuropathy. Gastrointestinal symptoms may include adverse effects such as nausea, vomiting, and diarrhea. Regarding the risk of renal system alterations, polyuria, polydipsia, and nephrogenic diabetes insipidus may occur. Lastly, the cardiovascular system may show signs of arrhythmia, low blood pressure, and in rare cases, septic shock [13].
In addition to the mentioned side effects, which can occur even within therapeutic levels of lithium, typical signs and symptoms of lithium intoxication should be carefully monitored. Plasma lithium levels above 1.2 mmol/L are potentially toxic, and in acute intoxication, plasma levels above 2.0 mmol/L can be fatal [14].
For the maintenance of lithium use, guidelines suggest a half life in the brain of approximately 24 hours, while the half life in plasma is 8 hours. Thus, despite a single daily dose of lithium being a viable option, most therapeutic guidelines recommend d ivided daily doses to maintain a stable plasma level. Therefore, initially, two or more daily doses may be applied to achieve a standardized serum lithium level over 12 hours, followed by a complete daily dose to enhance adherence and reduce the chance of increased urine volume. A therapeutic level of plasma lithium has been recommended as 0.5 1.2 mmol/L, and when initiating treatment, lithium levels should be checked in a steady state, i.e., at least five days after ingesting a specific dose, until two con secutive levels within the therapeutic range are established for the same dosage [10].
Although the specific therapeutic mechanisms of lithium in mood regulation have not been clarified, studies demonstrate that lithium exerts its mood stabilizing effects by acting on cellular targets and providing neuroprotective effects. It has been proven that the modulation of the GSK 3 pathway produces antagonistic effects on the depressive and manic components of bipolar disorder, as genes regulating GSK 3 have been implicated in the etiology of this psychopathology. Therefore, it is considered that lithium influences various neuroprotective pathways by increasing phosphorylated GSK3 β and inhibiting its action, improving the effects of excitotoxicity. Previous studies reported that the response to lithium treatment was predicted by the expression and phosphorylation of the GSK3β gene, and lithium induced increases in phosphorylated GSK3 β correlated with symptom improvement [15].
It is emphasized that the use of lithium in the treatment of bipolar disorder requires careful consideration of certain inherent risks associated with its ingestion, such as drug interactions, concerns about its narrow therapeutic range, adverse effects, and others that can be managed. Despite the effects present in its use, lithiumremains the safe st and most widely used first generation drug in the treatment of bipolar disorder, demonstrating viability in the risk benefit relationship.
Considering the studies already conducted and utilized in the literature review of this study, it is important to highlight the efficacy of lithium in individuals with bipolar disorder, especially in the prophylaxis of relapses in acute manic phases and suicide prevention. In this context, the review of this study on lithium is crucial for healthcare professionals and the families of individuals to understand the importance of this substance in maintaining mood stability in patients.
