Author(s): <p>Elizondo Martín</p>
Introduction: Non-alcoholic fatty liver disease affects 1/3 to ¼ of the world’s population. Currently this pathology is being redefined by using the acronym MALFD (Metabolic Dysfunction-Associated Fatty Liver Disease) and the possibility of new criteria for its diagnosis is being discussed.
Methodology: Prospective and descriptive studies carried out between July 2018 and June 2020 where the applicability of the new criteria in MAFLD diagnosis were valued. Patients with NAFLD (Non-alcoholic fatty liver disease) were enrolled in clinics specialized in this pathology.
Results: Out of 172 patients enrolled, 96.4% (this represents a total of 165 patients) presented obesity, were over weighted and or presented Diabetes Mellitus. The rest of the patients (a total of 7) presented high blood pressure and or dyslipidemia. Moreover, it was observed that the higher the obesity index the higher the prevalence of Diabetes Mellitus.
Conclusions: The criteria for the diagnosis of MAFLD are adaptable in patients with a diagnosis of NAFLD from the first consultation and allow the assessment of prognostic elements of the disease. This would allow us to intervene at very early stages which could impact patient’s prognosis
Non-alcoholic fatty lived disease (NAFLD) is considered the most common chronic liver disease, constituting a true epidemic. It affects between 20 to 30% of the world’s population and an exponential increase in its prevalence is expected, accompanying the epidemic of metabolic syndrome, obesity and diabetes mellitus (DM) [1, 2]. The prevalence in Uruguay is unknown [3].
In the last decade, substantial evidence has emerged stating
that NAFLD is a systemic disease. With a heterogeneous
presentation, where multiple factors such as demographic, genetic,
environmental, intestinal microbiota and metabolic dysfunction
interact. This evidence has raised the need to review both the
definition and the diagnostic criteria. The acronym MAFLD,
for Metabolic Dysfunction-Associated Fatty Liver Disease, has
been proposed, which rethinks this pathology with diagnostic and
therapeutic implications, and will allow a better understanding of
the role of metabolic dysfunction [4, 5].
We assess the usefulness of these new criteria at the time of
diagnosis and the interaction between them, as part of a preliminary
analysis of data obtained from the follow-up of patients in a
specific NAFLD polyclinic.
Prospective-descriptive study carried out between July 2018 and June 2020. Patients with a diagnosis of NAFLD were enrolled and assisted in the NAFLD polyclinic of the Liver Diseases Service in the Militar Hospital of Montevideo, Uruguay.
Patients of 18 years of age or older with a confirmed diagnosis of hepatic steatosis by abdominal ultrasound were included, once other etiologies of hepatic steatosis were ruled out and in the absence of alcohol consumption greater than 2 or 3 Units of Standard Drink according to sex (> 20 g alcohol / day women;> 30 g men). Percutaneous liver biopsy (PLB) was not used as a diagnostic criterion, nor to differentiate between steatosis and steatohepatitis.
Information related to sex, age and anthropometric measurements (height, weight, Body Mass Index (BMI) (weight / height2) was collected from the participating patients.
It was considered: normal weight BMI: 18.5 to 24.9 Kg/m2 ; overweight: BMI 25 to 29.9 Kg/m2 ; and obesity: BMI ≥30 Kg/m2 . Obesity was classified as grade 1, 2, and 3, according to BMI ≥30 to 34.9 Kg/m2 , 35 to 39.9 Kg/m2 , and ≥ 40 Kg/m2 respectively.
It was assessed how many patients met the new diagnostic criteria for MAFLD based on the presence of overweight / obesity, and / or DM. In those patients who did not comply with this, the presence of other elements of metabolic dysfunction such as alteration of the lipidic profile: TG> 150 mg / dL, HDL-cholesterol <40/50 mg / dL M/W or specific treatment, diagnosis of arterial hypertension (HT), or pre-diabetes (glucose> 100-125 mg / dl, Oral Glucose Tolerance Test 140-199 mg / dl or HbA1c 5.7-6.4%) were assessed. We do not have the rest of the criteria suggested by the authors at the time of the study, which were assessed in the evolution [4]. (Figure 1)
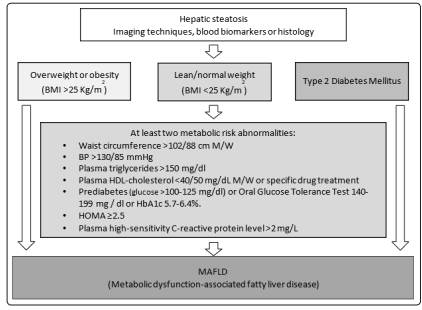
Figure 1: Diagnostic algorithm suggested by Eslam. J Hepatol. 2020 BMI (Body Mass Index), M (men), W (women), BP (Blood Pressure), HOMA (Homeostasis model assessment of insulin resistance score)
The PLB was not used as an initial diagnostic means, and was reserved as indicated by international guidelines, for patients with NAFLD with higher risk of having NASH and / or advanced fibrosis, or patients in which non-invasive methods of fibrosis measurement cannot be used to predict risk of NASH or advanced fibrosis, and / or to assess differential diagnoses or associated diseases [6, 7]. In these patients, PLB was performed during evolution; therefore, they are not expressed in this paper. For the descriptive analysis of the variables we used percentages of frequency and measures of central tendency. Statistical analysis was performed using the IBM SPSS Statistics ® operating system. This research was approved by the Scientific Committee on Research in Human Beings of the Militar Hospital.
A total of 172 patients were enrolled, of those 94 (54.7%) were women and 78 (45.3%) were men. The average age of the patients was 56 ± 12 years.
The BMI at the time of diagnosis was 31.7 ± 6.7 kg/m2 . Discriminated by BMI: 8% were normal weight (n 14), 24% (n 42) overweight, 68% (n 116) obese. No patient had a BMI less than 18.5 Kg/m2 . Of the subgroup of obese patients, 60% (n 70) had grade 1 obesity, 16% (n 19) had grade 2 obesity, and 23.3% (n 27) had grade 3 obesity (Figure 2) Of the total number of patients, 78 had DM (45.3%), of those 60.2% were women and 39.8% men. (Figure 3) The variables BMI and the presence of DM were related, and it was observed that the percentage of patients with DM is higher, the higher the degree of obesity. (Figure 4).
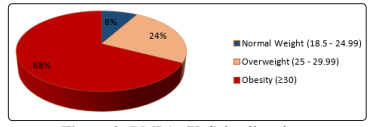
Figure 2: BMI (m/Kg2 ) in all patients
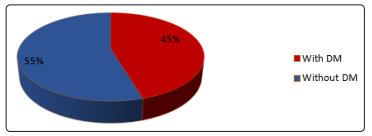
Figure 3: Presence of DM in all patients
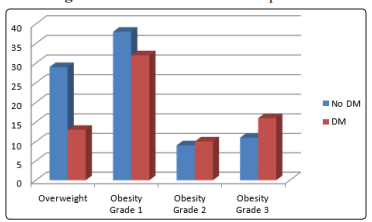
Figure 4: Increase in DM with a higher degree of obesity in NAFLD
A total of 96.4% of the patients fulfilled at least one of the factors needed for the new diagnosis of MAFLD: Overweight or obesity and / or DM. Among the 7 patients with normal weight and absence of DM, it was found that 4 of them had hypertension under treatment and / or alterations in lipid metabolism. Only 3 patients of the 172 did not have elements that allow the diagnosis of MAFLD.
Given the current and future impact of NAFLD on Public Health
worldwide, and the absence of recent data in Latin America, the
need to analyze local epidemiological data and establish diagnostic
algorithms and treatment options that adapt to the best scientific
evidence emerges. In order to early identify patients, and the
objective of establishing prevention, follow-up and treatment
strategies [8, 6].
The term NAFLD was first coined in 1980 by Ledwig and
his collaborators, and recently, with the advent and increasing
knowledge of this pathology, it has been interpreted that said term
does not reflect the most characteristic elements of the pathology
[9]. Experts have then proposed the acronym MAFLD. This new
definition could become a milestone in hepatology and allow a new
way of relating liver disease linked to fat deposit and metabolic
dysfunction.
The proposed diagnostic criteria are based on the presence of at least one of the following: overweight / obesity, type 2 DM or evidence of metabolic dysfunction (Figure 1), in this way the diagnosis is positive and not exclusive, in addition to removing the word alcohol from the definition with the difficulties it generatedin the interpretation of the disease by the patients [7, 10]. The data obtained in this communication shows that this new definition is applicable in daily clinical practice, since more than 96% of the patients meet these diagnostic criteria, using only anthropometric measures, comorbidities (DM and / or HT) and the lipid profile. A difficulty that arose when faced with the application of these diagnostic criteria was that in most patients we did not have the measurement of abdominal girth, nor did we have elements to complete the Homeostasis model assessment of insulin resistance score, nor the value PCR tests in plasma that are also part of the new diagnosis [4]. Despite this, only 3 of the 172 patients did not meet the diagnostic criteria outlined, which again supports the applicability of these criteria in clinical practice.
Another interesting fact of this preliminary analysis is the confirmation of the association between obesity and DM in NAFLD, since both pathologies were present in the majority of patients. On the other hand, an increase in the percentage of patients with DM was observed as the BMI increased in patients with NAFLD. And although it has not yet been assessed in this work, it is known that obesity and DM are associated with a higher prevalence of NASH and a greater progression of fibrosis in these patients. Therefore, assessing the presence of obesity and DM at the time of diagnosis is not a minor fact, given the prognostic impact it has [8, 5]. In addition, individuals with NAFLD and metabolic syndrome have higher overall mortality. For each component of metabolic syndrome, they have, their risk increases gradually.
NAFLD is associated with an increased risk of subclinical atherosclerosis, cardiovascular disease, type 2 DM, chronic kidney disease, liver, colorectal and breast cancer [8].
The data obtained suggest that the proposed criteria are adaptable and in most cases with great clinical applicability, and only a low percentage of patients may not meet them. It is important to think of NAFLD as a disease that exceeds the liver, with systemic involvement, subscribed in the context of other metabolic diseases (MS, DM, and dyslipidemia). In this way, early interventions could reduce cardiovascular risk and the events related to it, as well as reduce the progression of fibrosis and its complications, with great importance in mortality, especially in patients with less advanced disease [11, 12].
