Author(s): <p>Angeli Elaine A Pangilinan*, Luella Joy A Escueta-Alcos, Maria Teresita G Gabriel, Alexander R Castillo and Maria Francesca S Quinio Calayag</p>
Introduction: Basal cell carcinoma (BCC) is the most common cutaneous malignancy worldwide often occurring in sun-exposed areas. While the nodular variant accounts for the majority of cases, the adenoid type is extremely rare, comprising about 1.3% of all BCCs. Contrary to the typical presentation of BCC, adenoid BCC features a large sized lesion and a tendency to involve non-sun exposed areas such as the trunk. This case study presents a unique form of mixed superficial and adenoid BCC in a 57-year-old Filipino female.
Case Report: A 57-year-old female presented with a 2-year history of a slowly enlarging bluish-black plaque with rolled borders on the left flank with noted bleeding, pain, and pruritus. Dermoscopy revealed arborizing vessels, leaf-like structures, blue gray globules, and white streaks, consistent with BCC. Histopathology showed a diagnosis of a superficial and adenoid type of BCC.
Conclusion: Encounters with unusual forms of cutaneous carcinoma may arise in dermatologic practice. Dermoscopy serves as a powerful tool in identifying suspicious lesions and a pre-operative biopsy is done to correlate with the clinical diagnosis. Hence, the dermatologist will be able to decide the appropriate treatment option based on the clinical presentation and histopathologic type.
Basal cell carcinoma (BCC) is the most common cutaneous malignancy worldwide often occurring in sun-exposed areas. While the nodular variant accounts for the majority of cases, the adenoid type is extremely rare, comprising about 1.3% of all BCCs. Contrary to the typical presentation of BCC, adenoid BCC features a large sized lesion and a tendency to involve non- sun exposed areas such as the trunk and axilla. This case study presents a unique form of mixed superficial and adenoid BCC in a 57-year-old Filipino female.
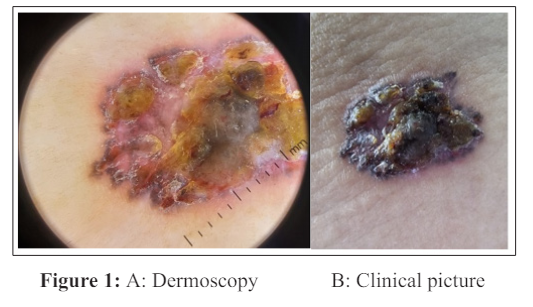
A 57-year-old Filipino female presented with a solitary, brown macule on the left flank with no noted pruritus, pain, bleeding, or discharge. No new medications were applied. In the interim, the lesion gradually increased in size evolving into a bluish black plaque with occasional pain and pruritus as well as minimal bleeding upon manipulation. 3 weeks prior to consult, the patient noted yellowish discharge on the affected area hence consult at our clinic. The patient had no loss of appetite or sudden weight loss, no difficulty of breathing, no arthralgia or limitations of movement. She has no history of comorbidities, malignancy, and allergies to food or medications. Clinical examination showed a solitary, well-defined, bluish black plaque with necrotic tissue and overlying yellowish crusts and discharge measuring 2 cm x 2 cm on the left flank (Figure 1). No lymphadenopathies were noted. Dermoscopy presented arborizing vessels, leaf-like structures, blue gray globules, and crusts (Figure 2).
With the clinical and dermoscopic findings, a primary impression of BCC with secondary bacterial infection was made. A bacterial gram stain culture and sensitivity (GS/CS) was done and a skin punch biopsy was requested once the infection is controlled. Empiric treatment with Cephalexin 500 mg/cap, 1 cap every 6 hours for 7 days and NSS compress for 7 days were given. For the GS/CS, yellowish discharge was collected on the lesion using a cotton pledget. Results showed gram positive cocci in clusters.
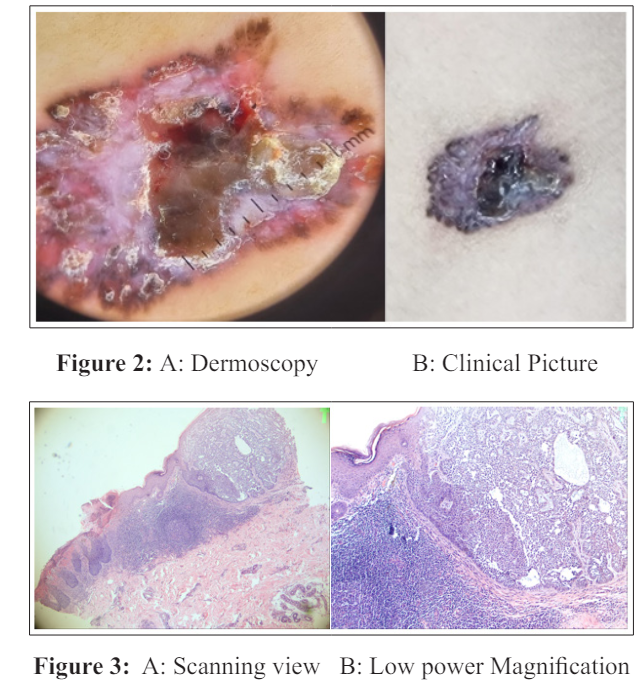
After treatment, the yellowish crusts and discharge resolved and the lesion presented as a solitary, well-defined, irregularly shaped, bluish black plaque with necrotic tissue measuring 2 cm x 2 cm on the left flank. Repeat dermoscopy revealed a clearer view of arborizing vessels, leaf-like structures, blue gray globules, and crusts. The white streaks were better visualized after the resolution of the yellowish crusts and discharge.
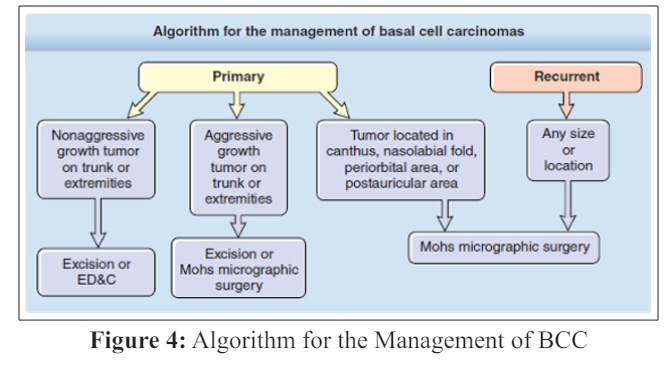
Skin punch biopsy was done showing two different histologic subtypes. On the left, there are numerous, small, basaloid lobules attached to the lower part of the epidermis, separated by normal epidermis and lymphocytic inflitrate, signifying superficial BCC, the second most common subtype of BCC. While on the right there are mucin-filled ductal spaces along with cribriform arrangement of basaloid cells which implies the diagnosis of adenoid variant of BCC which is a rare variant of BCC (Figure-3 A, B). These areas are separated by a monolayer of long basal cells arranged loosely perpendicular to a surface and parallel to each other, forming a peripheral palisade (Figure-3, B). BerEp4 expression was positive in nuclear and cytoplasmic staining of the normal adnexal epithelium of the patient. This distinguishes cutaneous BCC from other possible tumors.
A 57-year-old Filipino female presented with a 2-year history of a slowly enlarging brown macule evolving into a plaque on the left flank with bleeding upon manipulation, pain and pruritus. No past medical and family history of skin disease or malignancies were noted. There was no significant sun exposure and sunscreen use. Clinical examination showed a solitary, well-defined, irregularly shaped, bluish black plaque with necrotic tissue measuring 1.5 cm x 1.5 cm on the left flank with no lymphadenopathy. Dermoscopy revealed arborizing vessels, leaf-like structures, blue gray globules, and white streaks which are consistent with our working impression. Skin punch biopsy showed a mixed superficial and adenoid variant of BCC. The entire lesion was removed by standard excision.
A pre-operative biopsy is performed for confirmation of the clinical diagnosis and based on the risk will guide us as to perform standard excision vs. Mohs micrographic surgery. Punch biopsy was done instead of shave biopsy because the lesion is flat rather than mounded, shorter procedure time, and decreased cost [1]. Both the epidermis and dermis can be visualized and can confirm BCC and its subtypes. Biopsy revealed a mixed adenoid and superficial variant of BCC, which has a very small reported incidence of 1.3%. It has a tendency to involve unexposed parts. Our patient’s lesion was located at the trunk [2]. A histopathological picture similar to that of Adenoid BCC is Cutaneous Adenoid Cystic Carcinoma (CACC) which is a rare malignant neoplasm of the salivary gland that arises directly in the skin. The presence of a positive BerEp4 expression in our patient confirms our diagnosis of Adenoid BCC.
A pre-operative biopsy is performed for confirmation of the clinical diagnosis and based on the risk will guide us as to perform standard excision vs. Mohs micrographic surgery. Punch biopsy was done instead of shave biopsy because the lesion is flat rather than mounded, shorter procedure time, and decreased cost [1]. Both the epidermis and dermis can be visualized and can confirm BCC and its subtypes. Biopsy revealed a mixed adenoid and superficial variant of BCC, which has a very small reported incidence of 1.3%. It has a tendency to involve unexposed parts. Our patient’s lesion was located at the trunk [2]. A histopathological picture similar to that of Adenoid BCC is Cutaneous Adenoid Cystic Carcinoma (CACC) which is a rare malignant neoplasm of the salivary gland that arises directly in the skin. The presence of a positive BerEp4 expression in our patient confirms our diagnosis of Adenoid BCC.

Standard Excision is the treatment of choice for low-risk BCCs, and small BCCs less than 2 cm. 3- to 4-mm surgical margin are usually sufficient to achieve tumor clearance which was done in our patient [5]. Other treatment options include Mohs micrographic surgery, topical therapies (Imiquimod 5% cream and 5-FU cream), intralesional therapies, laser therapy, radiotherapy, electrodessication and curettage, cryosurgery, and photodynamic therapy [6].
Standard Excision is the treatment of choice for low-risk BCCs, and small BCCs less than 2 cm. 3- to 4-mm surgical margin are usually sufficient to achieve tumor clearance which was done in our patient [5]. Other treatment options include Mohs micrographic surgery, topical therapies (Imiquimod 5% cream and 5-FU cream), intralesional therapies, laser therapy, radiotherapy, electrodessication and curettage, cryosurgery, and photodynamic therapy [6].
BCC spreads to the lymph nodes, lungs, and bones. Metastasis can be monitored by checking the pelvic and lumbar lymph nodes. There is an extremely rare occurrence of metastasis, with incidence rates varying from 0.0028% to 0.55%. The pathways of tumor dissemination described are lymphatic or hematogenic, with the most common site of metastasis being lymph nodes, followed by the lungs. Risk factors of metastasis are (1) size, (2) history of previous radiotherapy, (3) local recurrence, (4) location in the central portion of the face or ears, (5) long period of evolution,(6) presence of perineural or perivascular invasion, and (7) immunosuppression. All of these were not seen in our case [7].
The prognosis for most patients with BCC is excellent. However there is still a decrease in the Quality of life of BCC patients due to concerns in scarring and disfigurement from treatment, anxiety, and fear of future skin malignancies. Patients with a history of BCC have a 3-year cumulative risk of 44% and 10-fold increase in BCC incidence compared with the general population. As a dermatologist it is important for us to advise our patients for the possibility of recurrence and how they can prevent it [6].
Encounters with unusual forms of cutaneous carcinoma may arise in dermatologic practice. Dermoscopy serves as a powerful tool in identifying suspicious lesions and a preoperative biopsy is done to correlate with the clinical diagnosis. Hence, the dermatologist will be able to decide the appropriate treatment option based on the clinical presentation and histopathologic type.
