Author(s): Taís Donha Yarid Angelieri, Lara Silva Miguel, Isabella Pedrotti Leme de Andrade, Gabriela Donha Yarid Angelieri, Matheus França Cunha and Joao Kleber de Almeida Gentile*
Amyand’s hernia is a rare condition consisting of the presence of the vermiform appendix within the hernia sac in the inguinal region. Despite not being frequent, or rarely reported, it deserves attention for proper care. Its involvement is more frequent in men of any age group and often goes unrecorded because the content of the hernial sac is reduced even before its identification.
Amyand‘s hernia (HA) occurs when the content of an inguinal hernia sac is a vermiform appendix, and is so called because it was first described by Claudius Amyand in 1735, when operating on an 11-year-old boy with this condition [1-4].
AH preferentially affects men, without particular age groups, there are cases ranging from newborns to 92 years old, but it can be up to 3 times more common in children than in adults due to the persistence of the peritoneal- vaginal conduit. It usually occurs on the right side, due to the normal anatomical position of the appendix, and is rarely found on the left side, but can be explained in cases of situs inversus, intestinal malrotation or mobile cecum [2-9].
A 39-year-old male engineer from São Paulo, SP, presented to the general surgery clinic with the complaint of a right inguinal swelling for the past 6 months, and a history of local pain on exertion with worsening pain over the past 3 weeks. Initial tests showed leukocytosis and ultrasonography of the inguinal region showed the presence of inguinal hernia with the presence of the appendix vermiformis within the hernia sac.
Physical examination showed an inguinal bulge to the right side during Landivar‘s maneuver with Valsalva, revealed it to be an indirect hernia. We opted for surgical treatment by laparoscopy on an elective basis, and performed an appendectomy in the first stage by the identification in the abdominal cavity inventory of the cecal appendage incarcerated in the hernial sac (Figure 1), and subsequently the treatment of the inguinal hernia with preperitoneal repair with placement of a protective mesh and closure of the peritoneum. The patient evolved asymptomatically, and was discharged from the hospital on the first postoperative day. He was evaluated at 7 and 30 days postoperatively without presenting any abdominal or infectious complications, and was discharged from the hospital cured.
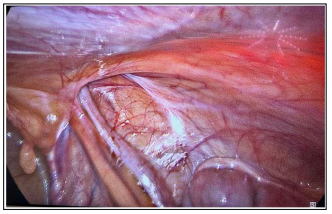
Figure 1: Indirect right inguinal hernia (lateral to the inferior epigastric vessels) with presence of the cecal appendage inside the hernia sac with signs of chronic incarceration
A hernia is a protrusion of a viscera or part of a viscera through the walls its cavity contains. It commonly occurs in the inguinal region, where the hernial sac may contain the omentum or small intestine. However certain unusual contents can be found, such as the bladder, a Meckel‘s diverticulum (Littre‘s hernia) or a part of the circumference of the bowel (Richter‘s hernia).
Amyand‘s hernia remains relatively unknown despite having been reported for nearly 170 years [10].The presence of the vermiform appendix (without or complications) within a sac is a rare event, comprising approximately 1% of all inguinal hernias [1-13].
Acute appendicitis in “Amyand‘s hernia” is even more controversial, being present in only 0.1% of cases, with a mortality of about 14 to 30% associated with peritoneal dissemination of the appendix contents [1-13]. It is usually caused by extraluminal obstruction due to pressure on the herniated neck rather than intraluminal obstruction from the appendix. Abu-Dalu and Urca suggested that the appendix becomes more vulnerable to trauma in “Amyand‘s hernia” and becomes trapped by adhesions when it enters the sac. Contraction of the abdominal muscles and other sudden increases in intra-abdominal pressure can cause the appendix to compress, resulting in further inflammation. Your blood supply may subsequently be cut off or significantly reduced, resulting in inflammation and bacterial overgrowth [4].
The clinical presentation is variable, ranging from asymptomatic to symptoms of irreducible and strangulated inguinal hernia [3,7,9,11].
Complaints usually include epigastric or periumbilical pain from sudden onset with localized tenderness in the right lower quadrant and inguinal edema, sometimes with a painful irreducible mass in the inguinal or inguinal scrotal region, with concomitant symptoms of fever, anorexia, nausea, vomiting and symptoms of mechanical intestinal obstruction. Typically, McBurney‘s sign is absent in these patients. In the case of an inflamed appendix, the condition can mimic orchitis or testicular torsion [1,5,7, 8,11,12].
Although not reported in the literature, perforation of an appendix inflamed inside the hernia can lead to thrombotic complications [8].
Due to the lack of guidelines and the rarity of cases, the diagnosis of Amyand‘s hernia is a real challenge, but it should not be overlooked when faced with presentations that fit the picture and often the diagnosis will only be made during the act surgical [1-3, 6-8,10,11].
Another factor that favors the intraoperative diagnosis is the fact that imaging tests are not always requested when simple inguinal hernia is suspected [7, 8]. In addition, several Amyand hernias end up going undiagnosed, since during elective surgery for an uncomplicated inguinal hernia, the herniated sac is reduced spontaneously, without identifying its contents [1].
Ultrasonography (USG) and computed tomography with contrast are very useful tools for the visualization of abdominal lesions, with USG being a useful and inexpensive method, with the presence of a non-compressible tubular structure within the hernial sac, which may present wall thickening and hyperemia. The topographic findings include tubular structure with blind termination inside the hernial sac, originating from the base of the cecum, wall thickening, hyperemia and strangulation of the periappendiceal fat [5,7,8,11]. Another diagnostic imaging method that has been used is multidetector computed tomography (MDCT), which more accurately identifies solid organ lesions and associated intestinal/mesenteric lesions, decreasing morbidity and mortality [4]. It is important to remember that the preoperative diagnosis based only on USG depends a lot on the technical skill of the operator, therefore it remains a relatively unreliable modalit [8]. Although difficult, one cannot stop thinking about the differential diagnoses, the main ones to be included are strangulated hernia, strangulated omentocele, Richter‘s hernia, testicular tumor with hemorrhage, acute hydrocele, inguinal adenitis and epididymitis, orchitis, testicular torsion, inflammation of the ovaries and inguinal lymphadenitis [3,4,6,11].
It is also important to remember that the major complications of Amyand‘s hernia are appendix perforation, anterior wall necrotizing fasciitis, and intestinal perforation [3,4,6,11].
The treatment consists of surgical management and there is still no agreement between the literature on the best conduct in repairing Amyand‘s hernia. The classic recommendation is to perform an appendectomy with herniorrhaphy in the presence of acute appendicitis, however some authors report the difficulty of deciding on the surgical approach for normal appendices, in young patients the appendectomy is performed to prevent a subsequent appendicitis. Other authors show the benefit of performing the appendectomy in order to avoid future operations and possible comorbidities, handling the healthy appendix can encourage inflammation and impair the blood supply, causing a secondary appendicitis [1,8,9,11-13].
Appendectomy in a normal-appearing appendix can lead to a high risk of intraoperative infection in a clean procedure turning it into a clean- contaminated surgery, since the procedure enlarges the deep annulus, leading to tissue weakness, making it impossible to use the appendix in urinary diversion, intestinal edema and biliary tract reconstruction, and in pediatric patients it is capable of compromising the immune development [7,8].
In cases of symptoms and signs of suspected strangulated hernia, laparotomy is required [9].
In cases of symptoms and signs of suspected strangulated hernia, laparotomy is required [9]. In the year 2007, Losanoff and Basson (Table 1) presented an Amyand hernia classification with their respective surgical recommendations, favoring intraoperative decisions, but there is still no agreement on how to deal with a normal appendix in pediatric patients [4, 6-8,11-13]. Rikki‘s modification, includes the presence of the normal or inflamed appendix within an incisional hernia, through the projection of the vermiform appendix, thus, it is divided into three more subtypes, 5a, 5b and 5c (Table 1) [7] .
Table 1: Losanoff and Basson Classification with Rikki‘s Modification
| Type 1 | Normal appendix within an inguinal hernia | Hernia reduction, mesh repairs, appendectomy in young patients |
| Type 2 | Acute appendicitis within hernia, no abdominal sepsis | Appendectomy through hernia primary repair of Hernia, no mesh |
| Type 3 | Acute appendicitis within an inguinal hernia, abdominal wall, or peritoneal sepsis | Laparotomy, appendectomy, primary repair of hernia, no mesh |
| Type 4 | Acute appendicitis within an inguinal hernia, related or unrelated abdominal pathology | Manage as type 1 to 3 hernia investigate or treat second condition as appropriate |
| Type 5a | Normal appendix within an incisional hernia | Appendicectomy through hernia, primary repair of hernia including mesh |
| Type 5b | Acute appendicitis within an incisional hernia, no abdominal sepsis | Appendicectomy through hernia, primary repair of hernia |
| Type 5c | Acute appendicitis within an incisional hernia, abdominal wall, or peritoneal sepsis or in relation to previous surgery | Mange as type - 4 |
Following the classification of Losanoff and Basson, Constantine et al illustrated 4 subtypes of Amyand‘s hernia by abdominal computed tomography, in which it is mainly used for the diagnosis of types 3 and 4 (Table 2) [11].
Table 2: Constantine Classification of Amyand‘S Hernia
| Type 1 | Appendix is normal |
| Type 2 | Enlarged and thickened appendix with inflammation of the surrounding fat |
| Type 3 | Excessive inflammatory changes are present, which could obscure the appendix |
| Type 4 | Related to other intra-abdominal findings |
Surgical repair with a prosthetic mesh is indicated in patients with a normal appendix, however it is contraindicated when the appendix is inflamed or perforated due to the high risk of contamination and postoperative infection, this is due to the high inflammatory response triggered by the mesh. Complete drainage of the wound associated with antibiotic therapy is recommended in the literature to reduce the risk of septic complications [3,4,8,12,13].
With the advancement of technology, minimally invasive surgery has become an effective and simple method for correcting hernias, making it possible to identify more severe intraperitoneal processes [14].
Amyand‘s hernia presents with the appendix trapped in the hernial sac in the inguinal region, being a rare event and difficult to diagnose, since the discovery is most often intraoperative. The surgical approach is controversial in the literature, leaving the choice of therapy and the best approach to the patient up to the surgeon‘s discretion.
