Author(s): Jing Chen*, Kappaganthu Venkatesh Prasanna and Yeow Leng Tan
Background: The ambulatory outcomes in traumatic conus medullaris syndrome (CMS) and cauda equina syndrome (CES) are important yet under-described.
Objective: This review aimed to determine the ambulatory outcomes of patients with traumatic CMS and CES, and to identify the clinical factors affecting these outcomes.
Methods: PubMed, EMBASE, CINAHL, and Cochrane databases were searched from database inception to August 2021. The searches were limited to articles in English language, human studies, and adult populations. Abstracts, letters, commentaries, editorials, conference posters, case series, case reports, and pilot studies were excluded. Two independent reviewers screened the studies, extracted relevant data regarding the ambulatory outcomes, and evaluated the risk of bias using the Joanna Briggs Institute critical appraisal checklist. If consensus could not be reached, a third reviewer arbitrated.
Results: Three articles with a total of 993 participants were analysed. The risk of bias was moderate in two studies and low in one study. The descriptions of ambulatory outcomes were heterogeneous. 111 out of 214 (52%) of the patients with traumatic CES achieved independent walking after rehabilitation. Data regarding walking ability in patients with traumatic CMS were lacking. Improvements in lower limb strength and functional mobility were similar in patients with traumatic CES and those with traumatic CMS. Early rehabilitation, less severe injuries, and lower neurological injury levels are associated with more favourable ambulatory outcomes. In view of the heterogeneity of ambulatory outcomes in the included studies, meta-analysis was not conducted.
Conclusions: The ambulatory outcomes of patients with traumatic CMS and CES were heterogeneous with more data available for CES. There is no evidence to suggest that traumatic CMS survivors have worsened motor and mobility prognoses than survivors with traumatic CES.
Conus medullaris syndrome (CMS) and cauda equina syndrome (CES) are two complex neurological disorders with overlapping anatomical and clinical manifestations [1-5]. The conus medullaris is the terminal portion of the spinal cord, and the cauda equina is a group of nerves and nerve roots that originate from the distal end of the spinal cord. As CMS and CES spinal cord injuries occur at overlapping anatomical sites, CMS and CES share common clinical features [1-5, 8].
These two similar clinical syndromes should be distinguished as it is believed that CES has a better prognosis than CMS. It is hypothesized that re-myelination is more effective in peripheral nerves than in central nerve fibres; therefore, CES, in which only lower motor neurons are affected, is expected to have a better prognosis than CMS, in which both upper motor neurons and lower motor neurons are affected. However, there are only few studies on this subject, with no systematic review [9-11].
The ambulatory outcomes of patients with CMS and CES have been under-described in previous studies, and the outcome measures reported are heterogeneous. Additionally, various outcome measures were used to assess walking, including the functional independence measure, Japanese Orthopaedic Association score, McCormick scale, and short-form health survey 36 [12-17].
As the data regarding the ambulation ability in patients with traumatic CMS and traumatic CES are not well summarized, a systematic review is needed. This systematic review summarized and evaluated the ambulatory outcomes of patients with traumatic CMS and traumatic CES, and to identify the potential factors that influence the ambulatory outcomes.
The reporting of this study followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis checklist [18]. A comprehensive electronic database search was performed in PubMed (Medline), EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Cochrane (CENTRAL) by two independent reviewers from inception until the end of August 2021 using a combination of search terms. The key search terms included CES, CMS, walking, recovery of function, and ambulation. The search terms were tailored to each database, as described in Appendix 1. A manual search of the reference lists of the included studies was conducted and associated systematic reviews and meta-analyses were identified. The results were limited to articles published in English.
Studies were included in this systematic review if they consisted of primary studies (prospective and retrospective cohort studies) of patients with CMS and/or CES, where trauma was the primary cause of injury. Eligible studies included adult patients with CES and/or CMS (≥19 years of age), and studies with walking ability, lower-extremity motor or functional recovery as outcomes.
Studies were excluded if they described nontraumatic causes of CES and/or CMS, included patients with pre-existing conditions that affected walking ability, or were abstracts, letters, commentaries, editorials, conference posters, case series, case reports, or pilot studies.
Two authors independently screened the search results for eligible studies, extracted the data into spreadsheets, and assessed the quality of the studies. Discrepancies in the ratings were resolved through discussion. If a consensus could not be reached, a third author was consulted.
The authors evaluated the risk of bias in the included studies using the Joanna Briggs Institute critical appraisal checklist for crosssectional studies [19, 20]. Eight items are included on the Joanna Briggs Institute checklists: the criteria for inclusion in the sample; the study participants and the setting described; measurement of the exposure; the objective, standard criteria used for measuring the condition; the identification of confounding factors; the strategies to deal with confounding factors; the measurement of the outcomes; and the statistical analysis.
Each component was rated as “yes,” “no,” “unclear,” or “not applicable.” A total of one to three “yes” scores indicated a high risk of bias; four to six “yes” scores indicated a moderate risk of bias; and seven or eight “yes” scores indicated a low risk of bias. Two authors independently evaluated the quality of each study. Disagreements regarding the methodological quality of the studies were discussed by two reviewers, and a third author was consulted if a consensus could not be reached.
In total, 707, 337, 130, and 53 articles were identified in the PubMed (Medline), EMBASE, CINAHL, and Cochrane (CENTRAL) databases, respectively. After duplicates removal, 1,152 articles were identified for screening. The titles and abstracts were screened, and irrelevant articles were excluded. A total of 52 articles were eligible for the full-text analysis. After a full-text review, 49 articles were excluded. The reasons for exclusion were as follows: case studies or case series (19 studies); non-traumatic causes of CMS or CES (17 studies); no ambulatory outcomes (11 studies); CMS/CES was not the primary diagnosis (one study); and pilot study (one study). Therefore, three studies were included in this qualitative analysis (Figure 1) [10, 21, 22].

The three included studies were published between 2007 and 2021, and the data were collected from 1992 to 2017 (Table 1). The three studies included in this analysis were a retrospective study comparing the functional outcomes in individuals with spinal cord injury syndromes, including central cord syndrome, Brown-Sequard syndrome, anterior cord syndrome, posterior cord syndrome, CES, and CMS conducted by [22]. a multicentre prospective cohort study that evaluated the neurological and functional recovery of patients with thoracic spinal cord injury, CMS, and CES conducted by Brouwers et al;10 and a prospective study evaluating the motor strength, walking ability, bowel and bladder functions, and factors associated with these outcomes in patients with traumatic cauda equina syndrome conducted by [21].

Most of the patients included in these studies had traumatic CMS or traumatic CES, though only 45.4% of patients with CES in the retrospective study had traumatic CES [22]. All three studies included patients with acute spinal cord injury. The diagnoses of CMS and/or CES were based on clinical findings assessed by qualified physicians in all three studies. The total number of patients in each study ranged from 175 to 1,573. The severities of CMS and CES varied according to the ASIA Impairment Scale [23]. The ambulatory outcomes assessed in the included studies are presented in Table 2.

CES: cauda equina syndrome; CMS: conus medullaris syndrome; FIM: Functional independence measure; SCIM: Spinal cord independent measure; LEMS: Lower extremity motor score
Of the three included studies, one by [21]. included the percentage of patients with traumatic CES that achieved ambulation [21]. This study included 214 patients with acute traumatic CES of varying injury severity. The percentage of patients with traumatic CES who were able to walk was 10% at rehabilitation admission and increased to 52% at discharge. In this study, independent walking was defined as a score of six or seven (modified/ complete independence) on the locomotion item of the functional independence measure, or a score of four to eight on the mobility for moderate distances on the spinal cord independent measure [24, 25]. No study included the percentage of patients with traumatic CMS that achieved ambulation.
One study compared the improvement in motor strength. The lower extremity motor score was used to assess the lower limb motor strength. Patients with traumatic CMS showed greater improvement in the lower extremity motor score than those with traumatic CES [10]. The difference in lower extremity motor score recovery was 4.68 points (range: 2.88–6.48 points, p<0.00). In this study, patients with traumatic CMS showed better improvement in lower limb motor strength than those with traumatic CES.
Different outcome measures, such as mobility sub-scores of the functional independence measure functional independence measure, indoor and outdoor mobility sub-scores of the spinal cord independent measure were described.
Functional mobility was assessed using sub-scores of the functional independence measure and spinal cord independent measure in two studies. In the study by [22]. the improvements in functional independence measure mobility scores, which reflect the degree of independence based on bed/chair/wheelchair, toilet, and tub/shower transfers, were not significantly different between patients with traumatic CMS and traumatic CES (11.17 vs. 9.73 points, p=0.06). In the study by [10] the spinal cord independent measure mobility sub-score analysis included indoor and outdoor mobility. The improvement in the mobility sub-scores of the functional independence measure were not significantly different between patients with traumatic CMS and traumatic CES. The indoor mobility sub-score of the spinal cord independent measure improved more in patients with traumatic CMS than in those with traumatic CES. The outdoor mobility sub-score of the spinal cord independent measure improved more in patients with traumatic CES than in those with traumatic CMS.
As these results are inconsistent, it is unclear whether patients with traumatic CMS or those with traumatic CES have a more favourable ambulatory prognosis.
Factors Affecting the Prognosis of Walking Ability Several factors contribute to the ambulation prognosis in patients with traumatic CMS and traumatic CES, including the neurological level of injury to the spinal cord. A higher neurological level of spinal cord injury suggests worse ambulatory outcomes. In the study by [22] patients with traumatic CES with a lower level (L3–S3) injury were more likely to walk at discharge than those with a higher level (L1) injury (89% L3–S3 vs. 35% L1, p<0.0001). [10] found that the lower extremity motor score 12 months after trauma was significantly worse in patients with thoracic spinal cord injury than in those with CMS and CES. This difference may have been because patients with thoracic spinal cord injury have the highest level of injury among these three conditions. Although patients with CES did not have greater improvements in the lower extremity motor score or spinal cord independent measure score than patients with CMS, this may be due to the ceiling effect of CES.
The severity of the injury is another factor affecting ambulatory prognosis. found that patients with more severe injuries (ASIA Impairment Scale A or B) were less likely to walk at discharge [21].
The waiting time from injury to rehabilitation was also identified as a factor affecting the ambulatory prognosis. Rehabilitation began at a median of 24 days after injury in the study conducted by [21] Patients with a shorter rehabilitation onset (within 24 days) were more likely to recover ambulation than those with a longer rehabilitation onset.
One study [21] had a low risk of bias, and two studies [22] had moderate risks of bias. The overall methodological quality of the included studies was moderate. The scores for each item of the Joanna Briggs Institute critical appraisal checklist for crosssectional studies are summarized in Appendix 2.
This systematic review included a comprehensive search on ambulatory outcomes in patients with traumatic CES and traumatic CMS. The reported descriptions of ambulatory outcomes in the included studies were heterogeneous [10, 21, 22]. Patients with traumatic CMS did not show poorer outcomes than patients with traumatic CES in terms of recovery of lower-limb motor strength and functional mobility. Factors affecting walking ability include the level and severity of injury, and time to rehabilitation.
Predicting independent walking following spinal cord injury is important to guide rehabilitation goal setting and strategy planning [26-28]. The findings of this systematic review indicate that more than half of the patients with traumatic CES are able to walk at the time of rehabilitation discharge. Although this result was derived from only one study including patients with traumatic CES [12], it suggests that the percentage of patients with traumatic CES who achieve ambulation is significant. The endpoint of the study, reporting a 52% ambulation rate in patients with traumatic CES, was ambulation upon discharge from rehabilitation as opposed to outcomes at a specific time point from the initial injury. Therefore, these results cannot be generalized to a different traumatic CES cohort, as the duration of rehabilitation varies at different rehabilitation facilities. No additional follow-up was conducted in the previous study; therefore, whether there was further improvement in ambulation and the final percentage of patients who achieved ambulation is unknown. This finding is consistent with that of a previous narrative review reporting that ambulatory potential is typically promising in patients with CES [29].
Two studies compared the outcomes of patients with traumatic CES to those of patients with traumatic CMS [10, 22]. These studies suggest that lower limb strength and mobility improvements are similar in patients with traumatic CMS and those with traumatic CES. reported that patients with CMS and CES exhibited similar functional independence measure functional outcome scores [22]. reported that patients with traumatic CMS have the greatest improvement in lower extremity motor score motor strength when compared to patients with thoracic spinal cord injury or traumatic CES, though the functional recovery on the spinal cord independent measure was similar in patients with thoracic spinal cord injury, traumatic CMS, and traumatic CES [10].
Previous studies suggest that lower motor neurons may have better regenerative capacity than upper motor neurons, and the higher neurological levels of injury were associated with poorer ambulatory outcomes [30, 31]. Therefore, traumatic CES is considered to have a better prognosis than traumatic CMS. The present finding that the recovery in traumatic CMS is not inferior to that in traumatic CES contradicts these previous findings. The similar improvement rates between traumatic CMS and traumatic CES patients may be due to several factors. First, the sample sizes of the studies included in this analysis are small. The study conducted by [22] included 14 patients with CMS and 44 patients with CES [22]. Subtle changes may be difficult to detect in studies with small patient populations. Second, traumatic CES patients presented with a good functional status at the initial state of the injury; therefore, the maximum improvement in the outcome measures, if achieved, did not affect the results. This is termed the ceiling effect.
In this systematic review, the factors that affect ambulatory outcomes include the neurological level, severity of injury, and time to rehabilitation. Higher levels of injury or more severe injuries are predictors of poorer outcomes, and these patients are less likely to achieve ambulation. Early rehabilitation is a positive prognostic factor for achieving ambulation. In the study by [10] patients with CMS had a more favourable recovery than patients with thoracic spinal cord injury [10]. The neurological level of injury plays a role in this recovery. reported that patients with traumatic CES who had less severe injuries were more likely to walk [21]. Moreover, based on a logistic regression model, a shorter rehabilitation onset (within 24 days) was significantly associated with walking ability at discharge from rehabilitation [21]. The findings in this systematic review are in agreement with those of other studies, as the overall rate of ambulation after spinal cord injury is dependent on the neurological level and severity of the injury, the extent of lower extremity motor function, and the patient’s age [30, 31].
This study has several implications. First, locomotor training to achieve independent walking should be included in rehabilitation programs for most patients with traumatic CES and traumatic CMS. A previous study reported that the types and duration of physiotherapy activities delivered during inpatient rehabilitation vary significantly among different levels of injury in patients with spinal cord injury [32]. Locomotor training can provide the appropriate sensory input to stimulate the remaining spinal cord networks and facilitate continued involvement [33, 34]. Second, the initial neurological level of injury and the severity of injury should be considered when predicting the functional recovery of patients with traumatic CMS and traumatic CES. Finally, early rehabilitation should be provided to optimize ambulatory outcomes.
This systematic review has several limitations. First, only three studies were included in this review; thus, information regarding more specific aspects, such as the walking ability in patients with traumatic CMS, is limited. Second, the heterogeneity of the study design and outcome measures used in the included studies render a meta-analysis difficult. There were not enough high-quality studies to assess the walking ability in patients with CMS or CES. Last, the diagnoses of CMS and CES in the included studies were based on clinical findings, without radiological confirmation. Although various measures were taken to avoid the inclusion of patients with mixed CMS and CES, the absolute accuracy of differentiating between these two cohorts is not possible without radiological confirmation.
The ambulatory outcomes of patients with traumatic CMS and CES were heterogeneous with more data available for CES. There is no evidence to suggest that traumatic CMS survivors have worsened motor and mobility prognoses than survivors with traumatic CES.
For the PubMed database search, the search strategies were as follows: Search on 4/August/2021
Search on 4/August/2021

For the Embase database search, the search strategies were as follows:
Search on 4/August/2021

For the CINAHL (CINAHL, OpenDissertations, eBook Collection, CINAHL Plus with Full Text) database search, the search strategies were as follows:
Search on 4/August/2021

For the Cochrane Central Register of Controlled Trials (CENTRAL) database search, the search strategies were as follows: Search on 5/August/2021

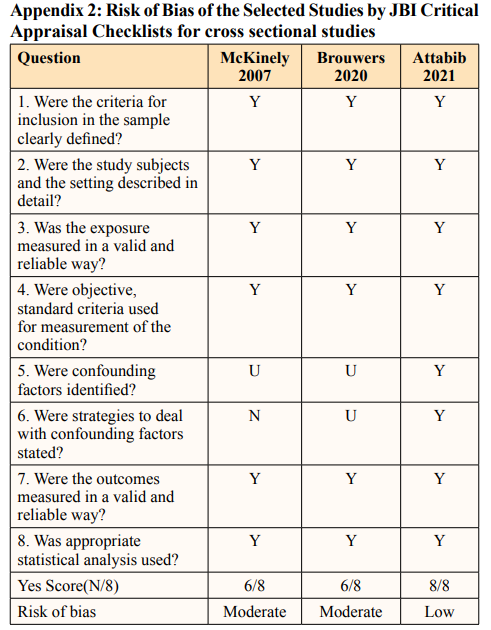
Y: Yes. N: No. U: Unclear
