Author(s): Blades CA*, Knowles GA and Francis W
The authors describe a potentially rare case of acute mesenteroaxial gastric volvulus in a pediatric patient. Gastric volvulus is a rare cause of non-bilious vomiting involving rotation of the stomach around its axis and has its peak incidence in the fifth decade of life. Acute gastric volvulus is a life-threatening, requires a high index of suspicion with prompt diagnosis and treatment to prevent significant morbidity and mortality.
In this case, a 6-year-old female child presented with nausea, vomiting, retching and epigastric pain. Abdominal distension and these non-specific symptoms prompted attempted passage of a nasogastric tube; further eliciting Bordchadt’s triad (epigastric pain, intractable retching and inability to pass nasogastric tube) which is specific for gastric volvulus. This was followed by imaging with abdominal ultrasound and CT scan, which revealed a malpositioned pylorus with tight stenosis giving a definitive diagnosis of mesenteroaxial gastric volvulus. The surgical procedure of anterior gastropexy without fundoplication along with gastrostomy was performed. The patient had an uncomplicated perioperative and post-operative course with full resolution of symptoms. It is hopeful that this case will serve as an educational platform for any future cases of gastric volvulus in the country and the region to help promote the early diagnosis and treatment that is needed for this rare but life-threatening surgical emergency.
Gastric volvulus (GV) is a pathological rotation of the stomach of more than 180° around its axis without obstruction and is a rare cause of non-bilious vomiting [1]. The diagnosis is challenging, and it is normally made on imaging or at the time of surgery. Without prompt diagnosis and treatment, GV is life-threatening can lead to severe complications including, obstruction, gastric ischemia and necrosis, perforation of the stomach and omental avulsion [2]. There are three types of gastric volvulus: organoaxial, mesenteroaxial or a combination of the two [3]. Organoaxial volvulus is the most common variant in the pediatric population [4].
We describe the case of a 6-year-old female with an acute history of vomiting which was subsequently diagnosed as mesenteroaxial GV on imaging. GV is often chronic, in contrast to our case, and can be asymptomatic. In our patient, the surgical procedure of de-rotation of the volvulus and gastropexy was performed via laparotomy with placement of a feeding gastrostomy tube. Post-operative course was uneventful, and the patient showed great improvement. Clinical index of suspicion in GV is always low given it’s unusual and rare presentation. We present this case because of its rare nature in our geographic location and in the general pediatric population. After conducting a thorough literary review, there has not been any published cases of GV in The Bahamas to date. To take it a step further, no documented pediatric occurrences have been found. Expanding beyond our geographic location, there have been only 65 cases of pediatric GV in the pediatric population published in English between 1979 and 2017 [5].
A 6-year-old female presented to our hospital with a 1-day history of abdominal pain, nausea and vomiting. The abdominal pain was localized the epigastric region, cramping in nature and nonradiating. The pain was exacerbated by vomiting and had no alleviating factors. The vomiting was post prandial; progressing to being unrelated to meals, and non-bilious. The parents denied any prior similar episodes and stated this was a first-time occurrence. They also denied any associated loose stools, fever or prior illness. There was no pertinent past medical or family history and immunizations were up to date.
On physical exam, the patient’s general condition was fair and she was in moderate painful distress. She had a blood pressure of 127/68 mmHg, temperature of 98.3°F, pulse of 105 beats per minute, respiratory rate of 19 breaths per minute and oxygen saturation of 98% on room air; all within normal range for the patient’s age. Mucus membranes were pink and moist, and pupils were equal and reactive to light. On auscultation, normal dual heart sounds heard with no murmurs noted, breath sounds were equal bilateral with no crackles or ronchi. The abdomen was grossly distended, soft but tender to palpation in the epigastric region, no organomegaly or masses were noted. Digital rectal examination was unremarkable.
Laboratory investigations included routine complete blood count with differential, a basic metabolic panel and liver function tests.
These tests revealed a normal complete blood count with the exception of an elevated platelet count of 478,000/uL and a normal white blood cell differential. Her basic metabolic panel and liver function tests also revealed no abnormalities.
An abdominal ultrasound and high-resolution CT with contrast of the abdomen and pelvis was then performed. Ultrasound showed gross gastric distension with a narrow pyloric outlet along with free fluid surrounding the spleen. A CT scan was advised to further evaluate the cause and site of obstruction. The CT scan showed a pylorus with tight stenosis that was malpositioned, posterosuperiorly to the left. A normally positioned but tight gastroesophageal junction was also noted with a grossly distended stomach. Subsequently, the diagnosis of mesenteroaxial gastric volvulus was then made and plans for treatment were devised.
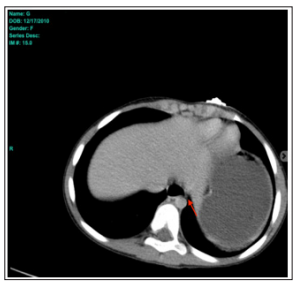
Figure 1: Axial Ct Showing Tight Ge Junction (Arrow)

Figure 2: Axial Ct Image Showing Gastric Volvulus

Figure 3: Saggital Ct Image Showing Malpositioned Pylorus

Figure 4: Coronal Ct Image Showing Grossly Distended Stomach
Attempts at passage of a nasogastric tube failed, the patient was resuscitated appropriately and further investigated esophagogastroduodenoscopy (EGD). Upon EGD the scope was unable to pass the fundus, 900mls of non-bilious content was suctioned and minimal areas of ischemia were found. Consent was then obtained for laparotomy. Laparotomy was performed via upper transverse incision and a distended, rotated stomach was found and delivered through the wound. All other abdominal and pelvic anatomy was examined and found to be grossly normal. The stomach was de-rotated, placed in the correction position and distal stomach pexied to the anterior abdominal wall. The fundus of the stomach was opened and a size 12F gastrostomy tube was placed and secured to the anterior abdominal wall. The procedure was uneventful with no perioperative complications. A diagnosis of mesenteroaxial gastric volvulus was confirmed on operation.
Gastric volvulus (GV) was first described in 1866 by Berti during an autopsy in the adult population and in the pediatric population in 1899 by Oltmann [4, 6]. In a systemic review conducted in 2018, there were 63 cases of gastric volvulus in the pediatric population documented in the English literature from 1979 to 2017, which can delineate that GV is a rare disease which also carries a high mortality rate [5]. GV is a rotation of the stomach, usually occurring with a large hiatal hernia but can also occur in patients without a hiatal hernia who have an unusually mobile stomach, as in our patient [1, 7]. The peak incidence has been found to be in the fifth decade of life and shown to be quite rare in the pediatric population [4]. The presentation of GV can be either acute or chronic. GV can be classified based on the underlying etiology as primary or secondary, based on the axis of rotation as organoaxial, mesenteroaxial or combined or based on anatomical location as either intraabdominal or intrathoracic [3]. Primary GV is the idiopathic subtype that occurs as result of abnormal attachment of the stomach like the patient in our case, neoplasia or adhesions. The stomach is fixed to the abdominal wall by four ligaments: the gastrocolic, gastrohepatic, gastrosplenic and gastrosplenic ligaments. These ligaments together with the pylorus and the gastroesophageal junction, prevent malrotation. Failure of fixation of the stomach can occur due to agenesis, elongation, or disruption of these gastric ligaments. Secondary GV can occur due to disorders of gastric function, anatomy or abnormalities of adjacent organs [3]. GV occurs due to secondary causes in about 70% of cases [8]. In our case, the gastric volvulus was of primary type without any associated diaphragmatic defect or paraoesophageal hernia. Organoaxial GV is a rotation of the stomach along its longitudinal axis more than 180 degrees, usually occurring acutely with an associated diaphragmatic defect. Whereas mesenteroaxial GV is less than 180 degrees rotation along the vertical axis with the antrum and pylorus lying anterior and superior to the gastroesophageal junction [2]. Mesenteroaxial volvulus is often recurrent and not usually associated with a diaphragmatic defect [7]. Organoaxaial volvulus occurs in up 60% of GV cases and results in an inverted stomach with the greater curvature of the stomach resting superior to the lesser curvature. Mesenteroaxial volvulus is less common and usually not associated with diaphragmatic defects. The third form is a combination of both organoaxial and mesenteroaxial with the stomach rotating about both axes [3].
Schematic representation of organoaxial (a) and mesteroaxial (b) gastric volvulus
GOJ = gastro-oesphageal junction,
GC = greater curvature,
LC = lesser curvature,
A = antrum [9].
The clinical presentation of GV depends on whether the onset is acute or chronic with both having distinctive patterns. Out of the 63 cases outlined in the systemic review of pediatric gastric volvulus, there were 37 acute cases and of those the most common symptoms were emesis/wretching followed by abdominal pain and/or distension [5]. According to the literature, the acute form, as in our case, presents with severe abdominal pain in the epigastric region accompanied by retching and/or vomiting. These features along with the inability to pass a nasogastric tube constitutes Borchadt’s triad (nonproductive retching, epigastric pain and distension, and the inability to pass a nasogastric tube) which is present in 70% of cases [10, 11]. Our patient presented with the classic features of Borchadt’s triad. However, in chronic cases the presenting symptoms may be nonspecific with dysphagia, mild abdominal pain and bloating, often being misdiagnosed as other gastrointestinal disorders [3]. These chronic nonspecific symptoms can go unnoticed and later transform into an acute volvulus needing emergent surgical management. Despite these presentations, GV can also be asymptomatic and discovered incidentally on radiologic imaging [3]. Acute GV is often associated with other anatomical defects, such as diaphragmatic hernia, eventration of the diaphragm, paraoesophageal hernia and congenital asplenia, unlike the patient in our case. Chronic GV is predominantly idiopathic in contrast such as the patient highlighted in a case report by Porcaro et al where a 16-month old female was found to have chronic GV without any other associated anatomical defects, which is noted to be the common occurrence documented in literature [4]. The patient presented by Porcaro had similar presentation and symptoms to our patient however it was over a longer period, leading to their diagnosis of chronic GV. Our patient, despite having acute GV, was not found to have any anatomical defects intraoperatively which sets this case apart from the findings noted in the literature.
As shown by a systemic review conducted in 2018 of pediatric gastric volvulus cases, diagnosing GV has proven to be difficult, given the rarity of the disease and requires a high index of suspicion as it is often not the first differential to be considered when a patient presents with abdominal pain associated with nausea and vomiting. X-rays may be diagnostic if there is a defect above the diaphragm showing a retrocardiac air-filled mass but the GV would still often be missed [5, 9-10]. Barium studies are regarded as the gold standard, especially in chronic cases associated with paraesophageal hernias, however, computed tomography of the abdomen is said to be the first line of investigation because it can not only confirm the diagnosis but also identify a transition point [4, 12]. The mortality for acute gastric volvulus has been reported to be as high as 30-50% with the major cause of death being strangulation leading to necrosis and perforation. However, this is greatly reduced with early diagnosis and treatment.
The management of GV depends on the initial presentation, the condition of the patient and the cause of the volvulus, if one is identified. The principles associated with the management of gastric volvulus include decompression, reduction of the volvulus, prevention of recurrence and repairing any predisposing factors. Acute GV is a surgical emergency and requires immediate surgical intervention to avoid ischemia and necrosis. There are many surgical operations that are available, however, the most frequently performed is an open surgical reduction with or without gastropexy after attempted gastric decompression via nasogastric tube to relieve the symptoms of gastric distension [3, 8]. Correction of the intra-abdominal factors that contributed to the volvulus are usually also included in the operation. In the pediatric population a gastrostomy is recommended, such as what was done for our patient, to further stabilize the stomach, maintain decompression and prevent recurrence of the volvulus [3, 13]. As with any open operation, there are risk associated, which prompted the development of more conservative approaches for GV, however, these are usually reserved for chronic GV and patients that are not surgical candidates such as the elderly. There are also several reports that describe a minimally invasive approach via endoscopic reduction and laparoscopy with insertion of a percutaneous gastrostomy tube, which has the potential to decrease the morbidity associated with an open operation [14]. However, patients with signs of acute peritonitis are better managed through an emergent exploratory laparotomy.
This case, being one of few described in literature for this region, illustrates the rare nature of mesenteroaxial gastric volvulus and the value of a high index of suspicion and imaging in its diagnosis in light of nonspecific symptoms. When gastric volvulus is suspected, prompt surgical management via emergency laparotomy is important to relieve symptoms, prevent organ necrosis and ultimately avoid mortality, which is up to 50% in untreated cases. This body of work should serve as an educational reference for any future cases that may be encountered in The Bahamas and the region with hopes that it will increase the index of suspicion to prevent any delays in diagnosis and treatment.
None declared.
Dr. C. Blades reviewed the literature and wrote the initial and final draft of the manuscript. Pre-operative assessment and general anesthesia were provided by Dr. M. Weech. Dr. W. Francis performed the operation assisted by Dr. G. A. Knowles. All authors contributed to the manuscript, and all read and approved the final version.
Dr. C. Blades assisted in the management of the patient, observed the operation and prepared the case report. Dr. W. Francis and Dr. G. A. Knowles are the surgeons who managed the patient and performed the operation.
Informed consent was obtained from this patient’s next of kin, for publication of this case report and any accompanying images. A copy of the consent is available for review upon request.
