Author(s): Bangoura Mohamed Saliou*, Guirassy Mariama II, Keita Doubany Mariame, Diallo Mamadou Abdoulaye and Toure Aboubacar
Acute intussusception is a rare manifestation in adults, most often of malignant tumoral origin occurring on a small intestine loop. Its presence in a pregnant woman with a complication such as peritonitis by ileal perforation is an extremely rare case. We report a clinical case concerning a 32-year-old woman, amenorrhoeic for 24 weeks, referred to the general and visceral surgery department of the Ignace Deen National Hospital for acute intestinal obstruction in pregnancy in whom, after performing an X-ray of the abdomen without preparation which revealed mixed hydro-aeric levels and a biological assessment, she was taken to the block, at the celiotomy purulent liquid flowed out and the exploration revealed a pudding of ileo-coeco-colic intussusception whose disinvagination revealed three ileal perforations with respective diameters of 1.5cm, 2cm and 3cm located respectively 10cm, 30cm and 50cm from the ileocecal junction with pre-perforation zones. We performed a resection removing the perforations followed by an end-to-side ascending ileocecal anastomosis. The post-operative course was marred by complications such as evisceration, disembowelment and the birth of a full-term stillborn.
Acute intestinal intussusception is defined by the penetration of an intestinal segment (invaginated loop) into the segment immediately adjacent to it (invaginating or receiving loop) by a reversal mechanism (like a glove finger) [1]. Its presence in adults, especially associated with pregnancy with a complication such as peritonitis by ileal perforation, is an extremely rare case, which can affect the maternal-fetal prognosis. The incidence of intestinal obstruction during pregnancy, in the most recent studies, was 1/1500 to 1/3000 pregnancies [2]. Diagnosis is difficult and often delayed because of misleading functional signs mistaken for vegetative signs of pregnancy. The physical examination may find a mobile sausage in the form of a mass in the flank, the right hypochondrium or anywhere else in the abdomen and bleeding on digital rectal examination. Ultrasonography plays an important role in diagnosis [3]. Surgery remains essential, and remains the method of choice regardless of the term of pregnancy to improve the prognosis and avoid serious complications. Through this work, we report our experience in taking an extremely rare case of intussusception in pregnancy complicated by peritonitis by ileal perforation.
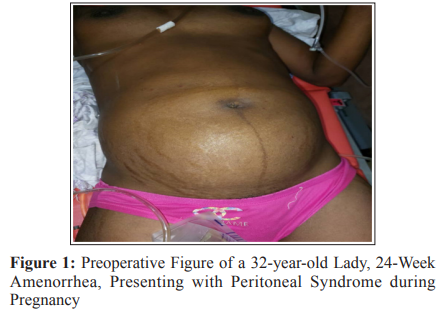
This is a 32-year-old patient, 24-week amenorrhea, received on February 21, 2023 for abdominal pain, vomiting, cessation of materials and gases and fever, all evolving for a week. HDM: the onset of the symptoms would be sudden, marked by the onset of stabbing abdominal pain initially sitting on the left flank, secondarily spreading to the entire abdomen, accompanied by postprandial vomiting, cessation of materials and gas, and fever. In front of this painting, she would have consulted in a health center where she would have benefited from a treatment made of injections whose names she does not know for 2 days. Without a favorable response, she decided to consult our department for support. No particular medical and surgical history, with gynecological history of four pregnancies, three parities, one living, two deceased, and one abortion. Date of last menstrual period unknown, amenorrhea about 6 months.
Patient conscious, cooperative, active attitude with a satisfactory general condition, hypocolored integuments and conjunctiva presenting the following parameters: TA=11/6, temperature= 38.5°C, pulse = 103 pulses/min, FR= 24 cycles/min. The abdomen increased in volume, symmetrical, participating in breathing. A generalized defense was noted, the prehepatic dullness preserved with a sloping dullness of the flanks. Audible intestinal peristalsis. Audible fetal heart sounds = 135 beats/ min. On vaginal examination: the vulva clean, the cervix short, closed, surmounted by an increased uterus, the finger cot comes out clean. On digitalrectal examination, the anal margin was free,the sphincter normotonic, the rectal ampulla empty, the Douglas fir bulging and painful. Examination of other devices and systems was unremarkable.
Thus we had carried out an x-ray of the abdomen without preparation which highlighted multiple mixed hydro-aeric levels associated with pelvic greyness; an obstetric ultrasound was also carried out which concluded with an evolutionary monofetal pregnancy of 24 SA + 3 days. A preoperative biological assessment was requested made of the NFS, glycaemia, blood ionogram, AgHbs, SRV, urea, creatine. GS/FR, TP, TCA which revealed anemia (THb=9.5g/l) which was corrected by the transfusion of a bag of packed red blood cells B+; hyperkalaemia, hypocalcaemia, hypomagnesaemia, hyponatraemia, lymphopenia and microcytosis which were corrected by the fundamental contributions
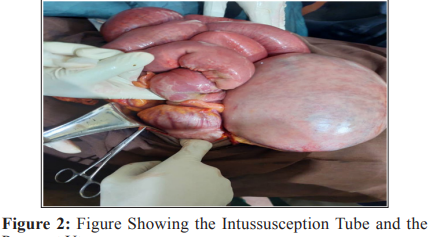
A tocolysis was made based on injectable salbutamol, six vials in glucose serum before admission of the patient to the operating room. Peroperatively, a median incision was made above and below the umbilical, at the celiotomy, purulent fluid and a globular pregnant uterus leaked. Exploration revealed an ileo-coeco-colic intussusception sausage whose disinvagination revealed three ileal perforations, the first measuring approximately 1.5cm in diameter located 10cm from the ileo-cecal junction, the second measuring approximately 2cm in diameter located 30cm from the ileocecal junction and the third measuring 3cm in diameter located 50cm from the ileocecal junction, with pre-perforation areas and pus in the parieto-colic gutters and in the Douglas fir. We had proceeded to the aspiration of 350cc of purulent liquid, to the resection removing the perforations, to the closure of the distal ileal end followed by an ascending end-to-side ileocolic anastomosis, to an additional appendectomy, toilet of the abdominal cavity using 4.5 liters of mineral water parietal closure plane by plane on a drain in the Douglas fir + dressing.

NB: five (5cc) of purulent fluid was sent to bacteriology and the surgical specimen was sent to the anapath.
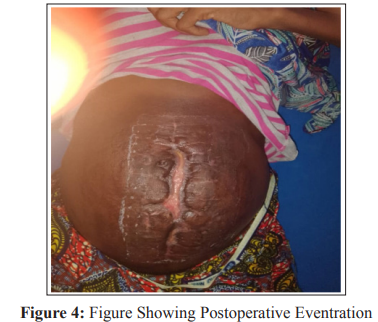
In the immediate postoperative period, she benefited from nifidine 20mg. Ceftriaxone 1g, metronidazole perf, alternating rehydration solutions and PPI were administered to him for 7 days. On her fourth postoperative day, she complained of cough and diarrhea which were managed with amoxicillin + clavulanic acid 1g + imodium 2mg + bronquiziadine. On the seventh postoperative day, the postoperative course was marred by complications such as parietal suppuration and fixed evisceration, which were managed with twice-daily dressings. A secondary suture was performed on her 15th postoperative day. On day 6 of the secondary suture, we observed a release of the suture threads exposing the intra-abdominal viscera. Faced with this picture of recurrent evisceration, she was taken back to the operating room where a cure for the eventration by aponeurotic approach in separate points was performed after excision of the edges of the wound and cleansing of the abdominal cavity with saline serum. On his 21 st day post hospitalization we received the result of the anapath which concluded in intestinal hemorrhagic infarction with necrosis of the intestinal mucosa plus peritonitis on intestinal intussusception and a submucous lipoma. During her hospitalization, the fetal heart sounds were perceptible varying between 130-135 fetal heart beats; she received three blood bags of isogroup globular concentrate, isorhasus B+, injectable spasfon 4 vials in 500ml of saline and two other obstetrical ultrasounds which did not note any particularity. The patient was released on her 75 th postoperative day with an improvement in her state of health in a postoperative hernia chart. At one month 15 days after her discharge from the hospital, she gives birth to a full-term stillborn.
Intussusception is rare in adults, especially in association with pregnancy. Its incidence varies between 1/5000 and 1/68000 according to the literature [4, 5]. In 2005, Choi S.A et al reported 6% intussusception of all bowel obstructions in pregnancy in France [6]. During pregnancy, intestinal obstruction may be related to the decrease in intestinal peristalsis and the increase in habitual constipation due to the progestogen impregnation favoring hypotonia of the intestinal smooth muscle and by topographic modification of the sequelae bands of a previous intervention following the development of the gravid uterus [7]. The majority of these intestinal obstructions (53-59%) are due to postoperative adhesions or bridles or episodes of pelvic inflammatory disease [8]. The other etiologies are represented by intestinal volvulus in 25% of cases, acute intestinal intussusception in 5% of cases, strangulated hernia in 1.4% of cases, and acute appendicitis in 0.5% of cases [7]. These occlusions generally occur between the 16th and 20th weeks of amenorrhea according to the literature; in our study, it occurred at 28 weeks of amenorrhea in a multiparous woman [3]. The diagnostic difficulty and the delay in the management of these occlusions can be linked to the often difficult and late clinical diagnosis of these pathologies, because their usual signs (pain, distension, vomiting, and constipation) are mistaken for sympathetic signs of pregnancy [9]. Physical examination may show a mobile sausage in the form of masse dans le flanc, right hypochondrium or anywhere else in the abdomen and a sign of bleeding on digital rectal examination. In our patient, the pudding was not palpated, probably because of the abdominal defense, and the digital rectal examination did not reveal rectal bleeding [3].
Imaging plays an important role in the diagnosis, of which abdominal ultrasound is the first-line diagnostic examination in the event of suspected intestinal obstruction [10]. It makes it possible to exclude an intestinal occlusion, to follow the evolution of the dilation of the intestinal loops, to detect the presence or the abundance of the intraperitoneal liquid and to appreciate the parietal thickening witness of a venous stasis, an ischemia or infarction in case of volvulus. Abdominal radiography without preparation is performed despite pregnancy in view of the high risks of morbidity and mortality from intestinal obstruction. It contributes little in the beginning forms, so it is recommended to repeat it at 12 to 24 hour intervals [2]. In our case, the plain abdominal X-ray was the first-line imaging and revealed mixed air-fluid levels and pelvic dullness. The biological examinations do not confirm the diagnosis, but are of great importance in the appreciation of the metabolic repercussions of the occlusive syndrome the ionic balance makes it possible to evaluate the state of hydration: Hypokalaemia and hyponatremia are often associated with lower intestinal obstruction, hypochloraemic alkalosis is found in case of vomiting, as for the renal assessment, it makes it possible to evaluate the secondary renal impact of dehydration [9].
Hyperleukocytosis is physiological during pregnancy, and can vary between 9000 to 12000 due to increased adrenocortical activity and therefore could be an unreliable indicator in pregnant women [7, 11, 12]. However, a significant increase in leukocytosis within a few hours should suspect intestinal obstruction [2]. In our patient, the biological assessment noted an ionic disturbance made up of hyperkalemia, hypocalcemia, hypomagnesemia, and hyponatremia; and abnormalities in blood count and formula made of anemia, lymphopenia and microcytosis. The treatment is medico-surgical whose medical treatment has no therapeutic purpose, it essentially prepares the patient for the surgical phase. As for surgery, it will improve the prognosis and avoid serious complications [3]. The preoperative preparation of these patients must require multidisciplinary management including an obstetrician, a resuscitator-anaesthetist and a surgeon in order to discuss the performance of prophylactic tocolysis, corticosteroid therapy for fetal maturation in the third trimester and the indication surgical. Surgical treatment must be undertaken within 72 hours to avoid major complications of necrosis, perforation and septic shock. Its main purpose is to remove the obstacle and sometimes treat the etiology in question [3]. An intestinal resection is necessary in 25% of cases [13]. Our patient underwent resection removing the perforations followed by an end-to-side ascending ileocolic anastomosis. According to Gurbulak the causes are specified intraoperatively or by histology. These may be Meckel’s diverticula, submucosal lipomas or other types [13].
Acute intussusception is a rare manifestation in adults, most often of malignant tumor origin occurring on the small bowel. Its presence in a pregnant woman with a complication such as peritonitis by ileal perforation is an extremely rare case with a high risk of maternal and fetal morbidity and mortality. The clinical diagnosis is often difficult and late and the treatment is essentially surgical.
The authors emphasize that there was no conflict of interest in the development of this work.
