Author(s): Aditi Raj, Nitin Gadgil and Anjali Amarapurkar*
Nodular regenerative hyperplasia and hepatocellular adenoma are two benign liver lesions with low risk of malignant potential. Nodular regenerative hyperplasia appears to be result of adaptive reaction to hepatic vasculopathy. Hepatocellular adenoma is associated with use of estrogen, anabolic steroids, metabolic disease and rarely vascular abnormality. We report an unusual case of a young female who presented with progressive dyspnoea, cough and edema. She succumbed to her illness within two days of her hospital stay. A medical autopsy was performed which revealed hepatocellular adenoma arising on the background of nodular regenerative hyperplasia along with pulmonary hypertension and intrapulmonary hemorrhage. Unusual case of nodular regenerative hyperplasia and hepatocellular adenoma associated with pulmonary hypertension where vascular pathology is suggested as a common event in their pathogenesis. Hence, it is advisable to rule out associated conditions with the help of imaging techniques in patients with pulmonary hypertension.
Nodular regenerative nodule (NRH) and hepatocellular adenoma (HCA) are rare benign liver lesions. NRH is characterized by regenerating hepatic nodules without fibrous septa with atrophy of intervening hepatic parenchyma. It is an adaptive response of hepatocytes to portal obliterative venopathy [1]. HCA is rare benign hepatic neoplasm usually associated with use of estrogen, anabolic steroids, metabolic disease or rarely vascular abnormality [2]. Combination of NRH with HCA occurring synchronously is extremely rare with occasional case report in literature [3,4] Here, we report unusual combination of NRH and HCA in a young female who succumbed to pulmonary hypertension (PH) and intrapulmonary haemorrhage.
A 21 years unmarried female presented to the hospital with cough and dyspnoea which progressed from grade one to four within 10 days. There were multiple episodes of vomiting with generalized oedema followed by unconsciousness. Her past history revealed amenorrhoea for three years with a negative urine pregnancy test. Patient was diagnosed with hyperprolactinemia. Serum prolactin level was 280ng/ml. She was treated with tablet Cabergoline (0.5mg) and Primolut N (10 mg). There was no history of connective tissue disorder, endocrine or cardiac pathology. At the time of admission routine laboratory investigations were within normal limits. Serum creatinine 1.9 mg/dl, total bilirubin 2.4mg/dl, AST 218 IU/ml and ALT 111 IU/ml. 2D echo revealed severe pulmonary artery hypertension. Patient died within two days of hospital stay due to pulmonary hypertension and intrapulmonary hemorrhage. A medical autopsy was performed. Systemic examination revealed voluminous and haemorrhagic lungs. Main pulmonary artery showed atherosclerotic plaque. (Figure 1A). Pituitary gland was normal with no evidence of hyperplasia or adenoma. There was no splenomegaly or oesophageal varices. Gross examination of liver showed multiple yellowish white tiny nodules ranging from 0.2 cm to 0.5 cm. Also noted was single large well circumscribed tan grey nodule measuring 2x1x1cm (Figure 1B). Adjacent liver parenchyma was noncirrhotic. There was no evidence of necrosis, haemorrhage or central scar. All other organs were unremarkable.

Figure 1: A ) Lung showing atherosclerotic plaque within pulmonary artery (white arrow)
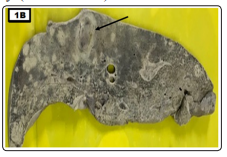
Figure 1: B) Liver showing small nodules of NRH and large nodule of HCA (black arrow)
Histopathology of diffuse tiny nodules revealed features of NRH exhibiting regenerating hepatocytes forming nodules without fibrous septa. Hepatocytes at the periphery of nodules showed atrophy. (Figure 2A). Microscopic examination of single large nodule showed partly encapsulated lesion with hepatocytes arranged in three to four cell thick trabeculae having bland morphology with no atypia or increased nuclear to cytoplasmic ratio. (Figure 2B). Few unpaired arteries were present within the lesion without interlobular bile ducts which was suggestive of HCA. (Figure 2C). Macrovesicular steatosis and inflammation were absent. Reticulin stain showed thick trabeculae without loss of reticulin network. Immunohistochemistry (IHC) for glypican 3 and CD34 was carried out to exclude the possibility of hepatocellular carcinoma. Ki67 mitotic index was <2%.
Sections from lungs revealed features of PH with extensive intrapulmonary haemorrhage. Many pulmonary arteries showed medial hypertrophy with few organizing thrombi and focal plexogenic pulmonary arteriopathy. (Figure 2D to F).
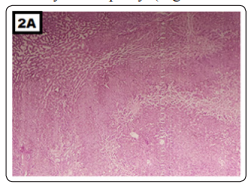
Figure 2: A) Nodules of NRH (HE 100X)
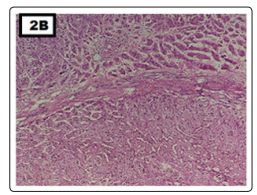
Figure 2: B) Partially capsulated HCA (HE 200X)
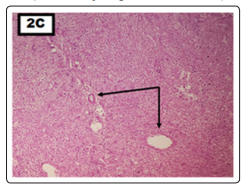
Figure 2: C) HCA with unpaired artery (HE 200X) (Two black arrows).
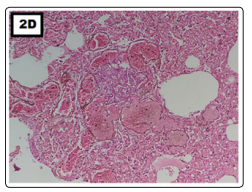
Figure 2: D) Lung showing plexogenic pulmonary arteriopathy (HE 200X).
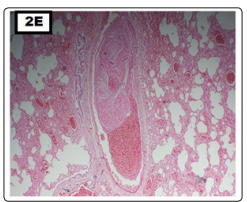
Figure 2: E) Pulmonary artery exhibiting thrombus (HE 200X).
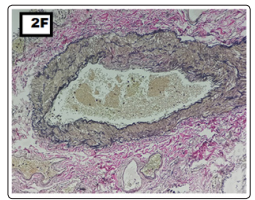
Figure 2: F) Elastic stain showing pulmonary artery wi
Majority of benign liver nodules remain asymptomatic and get diagnosed incidentally or at autopsy. NRH is characterised by transformation of liver parenchyma into small regenerative nodules which may progress to non-cirrhotic portal hypertension. Histopathology remains gold standard for diagnosis of NRH. The pathogenesis of NRH has not been clearly understood. Various theories suggested autoimmune, hematological, infectious, neoplastic or drug induced etiology [1]. Studies have shown role of drugs, such as steroids, anticancer agents, immunosuppressants, and contraceptives for the development of NRH. Wanless et al have reported phenomenon of portal obliterative venopathy which results in nodular transformation of liver (NRH) [1]. Nakanuma et al have shown obliterated portal venules in 107 liver biopsies of patients with NRH [5].
This patient presented with respiratory symptoms and was diagnosed as pulmonary arterial hypertension on 2D echo. Histopathology of lungs showed features of PH and presence of large thrombus. NRH was incidental finding at autopsy. Coexistence of NRH with PH is rare. Yutani et al in 1988 reported two autopsy cases of NRH associated with PH [6]. Portmann B et al reported a case of multifocal nodular hyperplasia of liver with noncirrhotic portal hypertension, later complicated by PH [7]. They have explained that prolonged exposure to blood born hepatotropic factors might have been responsible for nodular lesions in liver. Watabe H et al in 2006 reported three cases of NRH with connective tissue disease [8]. All three patients developed PH and subsequently NRH during their course of disease.
In addition to NRH, liver histopathology also showed presence of HCA. The stage at which both liver nodules appeared was not known. Coexistence of NRH with HCA is extremely rare with very few isolated case reports in literature [3,4]. HCA is known to occur in women of child bearing age and associated with use of estrogen, anabolic steroids, metabolic disease and rarely vascular abnormality [2]. This patient was diagnosed with hyperprolactinemia taking Primolut containing Norethisterone which might be one of the causative agent for HCA. However exact duration of treatment was not known. Hepatic vascular pathology could be common factor between NRH and HCA. Sempoux C et al have shown association of benign hepatic nodular lesions with hepatic vascular pathology [9]. Kobayashi S et al studied radiological and histopathological manifestations of hepatocellular nodular lesions concomitant with congenital and acquired hepatic hemodynamic abnormalities [10]. Recently in 2020 Bell P D et al reported HCA arising on the background of NRH in patient with systemic lupus erythematosus [4]. They have proposed that both nodular lesions could be attributed to hepatic vasculopathy secondary to SLE which is systemic inflammatory condition.
Our case reveals unusual relationship between PH, NRH and HCA. Pathogenesis may be either coincidence of pulmonary hypertension with liver nodules or could be multifactorial. Vascular pathology may be common factor for all three lesions. PH was serious complication associated with thromboembolic phenomenon and pulmonary veno-occlusive disease while alteration in hepatic microvasculature leading to NRH and HCA appears to be secondary effect.
We report very unusual case of NRH and HA associated with PH. Vascular pathology might be common event in this case for all three lesions. Hence, in patients of PH it is advisable to rule out associated conditions with the help of imaging techniques.
Conflict of interest: No commercial affiliation or conflict of interest.
Acknowledgement: NIL
