Author(s): Dr Bharti Sharma
The case report of an unusual case of human monkeypox with atypical epidemiology, unknown transmission route and unusual as well as rare ocular involvement with severe symptoms is presented in this case study.
Dear Editor, I want to report a very significant case report of a unique case of human monkeypox infection that presented with unusual features in terms of epidemiology, transmission and clinical symptoms. This case report indicates an evolving form of the human monkeypox infection that requires a broad strategy for testing and diagnosis of monkeypox in this new form.
A 36 year old male consulted for the appearance of rashes in the anogenital regions, right eyelid margin lesions with discharge, several papular lesions in the left eyelid with progressive conjunctival and peri-orbital involvement. The patient has severe pain in both eyes, significant light sensitivity, vision impairment and also presented with asthenia, headache, myalgia, lymphadenopathy, chills and sweats but had no fever at all. The patient was not gay or bisexual. He had no history of travel to any endemic country or any contact with a confirmed or diagnosed monkeypox patient. The patient did not have any history of smallpox vaccination, incidents of any autoimmune disease or HIV (human immunodeficiency virus) infection.
The patient was diagnosed positive for the monkeypox virus using a cutaneous polymerase chain reaction (PCR) swab from conjunctival PCR swabs and the anogenital rash. The viral load was similar in the conjunctival secretions and the cutaneous lesions (29.5 vs 27.3 [cycle threshold] respectively). Three days into hospitalization, the patient developed a mild fever which lasted just 24 hours. The patient continued to present with photophobia and severe eye pain with anogentital rashes over a period of 6-9 days. There was no recorded development of paronychia and lymphangitis of the anogenital lesions or any subsequent incidence of cellulitis in this case. This is very different from the clinical symptoms that have been documented in many cases of the human monkeypox 2022 outbreak [2, 3]. The patient was treated using oral as well as intravenous tecovirim. Ocular therapy included administration of topical trifluridine, antibacterial drops and an ointment of paraffin and retinol palmitate. The patient description and hospitalization treatment summary is shown in Table 1 below.
| Patient Characteristics | |
|---|---|
| Age (years) | 36 |
| Medical History | No HIV, no autoimmune diseases, not gay or bisexual, no smallpox vaccination, no known contact with a confirmed monkeypox case |
| Symptoms | |
| Fever | NA |
| Number of skin lesions | 30-42 |
| Lymph nodes involvement | Yes |
| Cellulitis | NA |
| Pustular papules | Present on one eye |
| Headache | Present |
| Reason for Hospitalization | |
| Ocular symptoms with significant pain |
Present |
| Paronychia | Present |
| Myalgia | Present |
| Light sensitivity & vision impairment |
Present |
| Lymphadenopathy, genital rash, chills and sweats |
Present |
| Surgical Management | NA |
| Antibiotics | Antibacterial drops |
| Ocular therapy | Topical trifluridine, antibacterial drops and an ointment of paraffin with retinol palmitate |
| Pain killers | Opioids with Acetaminophen |
| Other specialists for treatment | Ophthalmologist |
| Length of hospital stay (days) | 18 |
| Follow up at 2 weeks | No progression to permanent sequelae in the eyes |
Previous outbreaks of human monkeypox (involving the Congo Basin virus clade or the West African virus clade) have been documented as having a typical clinical onset with fever, rash and subsequent lymphadenopathy [1]. The patients in most cases had documented travel history to endemic nations or confirmed contact with a positive monkeypox case. The known, usual complications involved development of pneumonitis, encephalitis, visionthreatening keratitis or concurrent development of secondary bacterial infections [2-6]. The 2022 outbreak of monkeypox in various countries involved gay, bisexual or other males and some did have travel histories to endemic countries [6-9].
What is striking in this reported case is that the genital rash resolved after 8 days with the unusual rash initiation before fever, the continued presence of ocular lesions at multiple stages of the infection and the negligible febrile viral prodrome phase. Atypically, the ocular symptoms like the periorbital lesions continued to remain severe for 15 days before ocular symptoms and lesions as well as visual impairment were resolved. The patient was discharged after 18 days from the onset of the ocular symptoms and the anogenital rash. The patient did not suffer from any permanent eye damage or vision impairment despite the severe ocular involvement of both the eyes in the monkeypox infection. Further follow up with the patient after two weeks also confirmed that there was no progression to permanent sequelae in the eyes. This case has shown very unusual epidemiology and clinical symptoms and the potential of transmission via eye contact due to the detected viral loads.
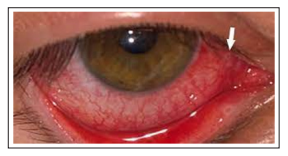
Figure 1: Clinical Symptoms of the Patient in the Eyes at Consultation
The case report presented above shows that the human monkeypox infection may be circulating in this new form with unusual clinical symptoms, epidemiology and transmission routes. As such, clinicians need to be vigilant and follow wider monkeypox case definitions and the possibility of early ocular involvement as a symptom of severe infection also. As suggested by some previous literature, there is need to revisit the currently accepted case definition being used by clinicians in all countries for a possible human monkeypox case as this follows the typical viral prodrome duration and clinical phases with the known transmission routes and usual epidemiology. The need to take into consideration atypical transmission and clinical symptoms is vital as it will help clinicians to test for atypical suspected monkeypox cases in the future. Thus, there is need to have broad case definitions for possible human monkeypox cases with rare clinical symptoms and transmission.
Data Availability Statement: Data available in the article
Funding: Not applicable
Conflict of Interest: No conflicts of interest to disclose
