Author(s): <p>Sheena Kaur Samagh and Nikhil Kumar Gautam*</p>
Oral sub mucous fibrosis (OSMF) is a chronic, insidious, disabling disease of oral mucosa, oropharynx, and rarely, the larynx affecting millions of people worldwide with a prevalence rate of 0.4% in Indian rural population. It results in difficulty in the mouth opening and can be disabling to the patient. It needs a timely diagnosis and thus appropriate treatment can be administered depending on the degree of involvement. A case of oral sub mucous fibrosis occurring in a 55 year old male patient is presented in this article.
Oral submucous fibrosis (OSMF) is a potentially malignant disorder caused by chewing of betel quid. It results in progressive inability to open the mouth [1,2]. OSMF has been predominantly reported among Indians living in India as well as outside, to a lesser extent among other Asiatics and, sporadically, among Europeans [4,5]. With a reported prevalence ranging up to 0.4% in Indian rural populations, several million individuals are estimated to suffer from this malady [4,5,6]. It has a malignant transformation rates as high as 7.6% and a relative risk of 397.3 for oral cancer development compared to individuals with tobacco habits but without any precancerous lesion or condition [5,7]. The present case report describes a case of OSMF in a 35 year old male patient.
An 55 year-old male patient brought to the department with complaint of inability to open the mouth and burning sensation in mouth on having spicy food since last two months. There was a history of eating arecanut 5-6times per day for the last one year. Patient had sunken cheeks with reduced cheek blowing capacity (Figure 1) and tongue protrusion and restricted mouth opening. On Oral examination, pale blanched appearance of left buccal mucosa extending from the retrocommisural area up to the retro molar area anterior posteriorly and superior inferiorly from approximately 5 mm above and below the line of occlusion. Marble stone appearance of mucosa was also observed with reduced inter-incisor distance (IID) of 1.5 cm and generalized tobacco stains on teeth and hard palate with decreased elasticity. Vertical bands were palpable in the buccal mucosa with respect to left posterior molar region on right side and the retro molar area. Circular band were palpable with respect to the mandibular labial mucosa. Based on the clinical findings a provisional diagnosis of Oral Sub mucous Fibrosis was made. Incisional biopsy was taken and microscopic findings (Figure 2) revealed a stratified squamous parakeratotic epithelium which was atrophied in certain areas with loss of rete ridges. The underlying connective tissue revealed dense bundles of collagen fibres merging with the muscle layer in the deeper connective tissue. Diffuse mild inflammatory infiltrate was seen. The histopathologic features were suggestive of Moderately Advanced Oral Sub mucous Fibrosis. On the basis of Histopathological findings a final diagnosis of Group III (moderately advanced) Oral Sub mucous Fibrosis was made.
Oral submucous fibrosis is regarded as a collagen metabolic disorder with an overall increased collagen production and decreased collagen degradation resulting in increased collagen deposition in the oral tissues, and fibrosis due to alkaloid exposure as a result of exposure to AQ [8,9]. Oral Sub mucous Fibrosis was first described by SCHWARTZ in 1952 among five East African women of Indian origin. This was followed by the first description of this condition in India in 1953 in quick succession [10,11]. Oral submucous fibrosis is seen predominantly in Asians who chew betel nut quid or its variants such as gutkha (mitha pan), kiwam, zarda and pan masala. The easy availability of packaged dried product such as gutkha, is increasing the incidence of this condition, as it consists of a greater dry weight of areca nut quid along with other OSMF producing ingredients than the traditional quid rolled in betel leaf (paan). Only betel nut chewing does not cause OSMF, contribution of other ingredients like slaked lime is more important in the causation of OSMF [9]. Areca nut chewing, smoking tobacco, smokeless tobacco and hypersensitivity to chilies are the causative agents in genetically predisposed patients [12]. OSMF mostly affects the buccal mucosa, lips, retro molar areas, soft palate. It is a chronic condition characterized by mucosal rigidity of varying intensity due to fibro-elastic transformation of the juxta-epithelial layer. This leads to restricted oral opening; when the tongue is involved, its protrusion may be impaired [4,5].
Early lesion present as a blanching of buccal mucosa, imparting a marble-like appearance but later lesions reveal palpable fibrous bands rendering the mucosa pale, thick and stiff. This leads to progressive inability to open the mouth, burning sensation, pain, dysphagia and finally hearing loss [12]. Most affected individuals report a burning sensation of the oral mucosa aggravated by spicy food. The presence of palpable fibrous bands is a requisite diagnostic criterion for this condition. Iron and vitamin B12 deficiency has been associated particularly in conjunction with other factors [13,14]. Oral submucous fibrosis can be seen at any age, but is rare in young children. The predominant age group affected is 20-40 years. Compared to traditional betel nut quid, gutkha chewing tends to begin at a younger age and has a shorter time to the development of disease, so cases of OSMF have begun to appear in younger age group.
OSMF is a potentially malignant condition [11]. The malignant transformation rate is found to be 4.5-7.6% [15]. The possible precancerous nature of OSMF was first described by Paymaster who observed the occurrence of squamous cell carcinoma in onethird of his patients with the disease [15,16].
The treatment of OSMF depends on the degree of involvement and timely diagnosis. Patients with OSMF need treatment for trismus correction, reconstructive surgery for any simultaneous oral malignancy [14].

Figure 1
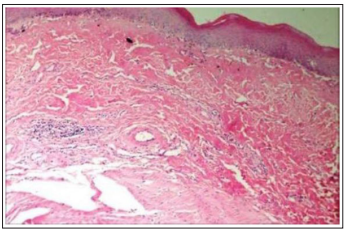
Figure 2
OSMF is a potentially malignant disorder, which requires close monitoring and follows up. Areca nut has been imposed as one of the initiating factors for the disease causation. Various treatment modalities are present and are used as per the stage of disease. This case report deals with the presentation of the condition in a 55 year old male patient with a chronic habit of arecanut. Early diagnosis and emphasis on patient counseling especially in a youth along with the appropriate treatment can help improve the condition drastically
